Anatomy and Function of the prostate
(Compiled July 2018)
What is it?
The prostate is a small gland about the size and shape of a walnut. It is part of a man’s internal sex organs. All the sex organs play a role in reproduction. The prostate generally increases in size as men age.
Where is it?
It is situated under the bladder and surrounds the urethra which is the tube that transports urine from the bladder to the penis where the urine is released through the ureter. This why problems with the prostate often affect the ability to urinate, causing what doctors call (urinary symptoms).
The rectum sits directly behind the prostate. This means that a part of the prostate can be felt if a finger is inserted up the rectum. (digital rectal examination) or the “finger” test. The tube that carries the semen from the testicles feeds into the ejaculatory ducts which then connect to the seminal vesicles which are just above the prostate. When prostate cancer spreads it often spreads first into these structures that surround the prostate. The prostate has gland tissue and smooth muscles fibres which help it to contract when a man ejaculates. The prostate is surrounded by a loose capsule which is connected to sheaths of pelvic muscles. Before 1981 surgeons were not aware of the nerve bundles towards the back and sides of the prostate that play an important role in erections. The identification of these nerves led to the first “nerve sparing” prostatectomy in 1982. Knowing where these nerves are situated has made a big difference to minimising erectile dysfunction in men who have had a prostatectomy.

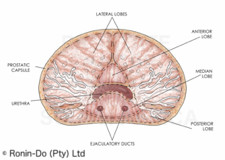
Until a few years ago, doctors described the different parts or areas of the prostate as lobes (see illustration below). One method of staging prostate cancer was to determine which lobes had been affected by cancer cells.
A more up-to-date way of describing the different areas of the prostate is the Zonal System. (See illustration below). 80 to 85% of prostate cancers start in the peripheral zone.

What does it do?
The prostate gland produces prostatic fluid which makes up about 15 to 30% of the semen or ejaculate. The average amount of semen ejaculated is 3.4ml which is less than a teaspoon full. Sperm make-up only 1 to 5% of the total volume of the ejaculate. The secretions from the seminal vesicles make-up the majority of the ejaculate. The secretions from the various glands that help to produce semen all assist with nourishing and protecting the sperm so that they can survive and impregnate an egg in the process of reproduction.
References
(1) Nicholas J., Primer on Prostate Cancer-2014, Springer Healthcare 2014.
(2) William K, Hurwitz M, D’Amico AV, et al. Biology of Prostate Cancer. Holland-Frei Cancer Medicine. 6th edition. Hamilton (ON): BC Decker; 2003. Available from: https://www.ncbi.nlm.nih.gov/books/NBK13217/
(3) Owen DH., Katz DF. A Review of the Physical and Chemical Properties of Human Semen and the Formulation of a Semen Simulant. J Androl 2005;26:459–469.
How common is Prostate Cancer in South Africa?
(Compiled February 2019)
According to Globcan, prostate cancer is the most frequently diagnosed cancer among men in over one‐half the countries of the world including the Americas, Northern and Western Europe, Australia/New Zealand, and much of Sub‐Saharan Africa. It is the leading cause of cancer death among men in 46 countries, particularly in Sub‐Saharan Africa and the Caribbean. (1a)
Although there are no reliable statistics on the incidence of prostate cancer amongst South African men, it is possible to get an idea of how common prostate cancer is in South African men by looking at the data from countries where men have reasonable access to screening for prostate cancer and where there is a significant population of black men with African ancestry. (Race is a proven risk factor for prostate cancer with black American and Jamaican men of African descent having the highest recorded rates of prostate cancer worldwide). (2a)
In the USA approximately 11.2 percent of all men will be diagnosed with prostate cancer at some point during their lifetime according to The SEER data from the National Cancer institute. (3) However if we compare the rates of prostate cancer in white vs black African American men there is a significant difference. It is estimated that 1 in 6 black African American men will be diagnosed with prostate cancer in their lifetime compared with 1 in 8 white American men. (2b) If we look at the data from 2008 to 2012 it showed that Black African American men had a 70% greater chance of being diagnosed with prostate cancer than white American men. (2c) They were also more than twice as likely to die from prostate cancer as their white counterparts, although this has improved in recent years.(2d)
One major advantage that black American men have over black South African men is that they are more likely to be diagnosed when the cancer is at a local or regional stage.(2e) (In other words, before it has spread to other parts of the body). This means that after 5 years most of these men will still be alive. In South Africa, the majority of black men will only be diagnosed when the cancer has spread, this is called metastatic prostate cancer and it is incurable.4 This means that after 5 years only about 30% of these men will still be alive. (5) Black African men from Southern Africa appear to have an additional disadvantage in that they present with significantly more aggressive prostate cancer than African Americans. (1b)
According to Prostate Cancer UK, 1 in 8 men will be diagnosed with prostate cancer at some point in their lives(6a) and for black British men of African descent 1 in 4 men can expect to be affected. (6b)
We recommend that black South African men consider screening from the age of 40 and that other ethnic groups start screening from 45.
Prostate cancer is more common in men with a family history of prostate cancer. If you have a family history of prostate cancer you are twice more likely to get prostate cancer. Having a brother with prostate cancer appears to put you at a higher risk than if you have a father with prostate cancer. The more family members affected by prostate cancer the more likely you are to get it. (7)
There is some evidence showing that prostate cancer is also more common in men who have a first degree relative who has been diagnosed with breast cancer, particularly when the breast cancer was diagnosed before the age of 50. (8) Men who have a daughter who has been diagnosed with breast cancer have a higher risk for aggressive prostate cancer.
We recommend that men with a family history of prostate or breast cancer in a first degree relative consider screening from the age of 40.
Conclusion
- Based on current USA and UK data and various clinical studies:
- About 1 in 8 to 1 in 9 white South African men are likely to be affected by prostate cancer.
- As life expectancy amongst black South African men increases, between 1 in 4 and 1 in 6 men are likely to be affected by prostate cancer. Black men are more likely to get prostate cancer at a younger age and a more aggressive type of prostate cancer.
- Prostate cancer is more common in men with a family history of breast and prostate cancer.
- Men who are at increased risk for prostate cancer because of their race or family history should consider screening for prostate cancer from the age of 40
- All other men should consider screening from the age of 45
Ref 1 Bray F et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca: A journal for Clinicians. Vol 68 no. 10 Nov/Dec 2018 Available at: https://onlinelibrary.wiley.com/doi/full/10.3322/caac.21492
Ref 2 Ref DeSantis CE, Siegel RL et al. Cancer Statistics for African Americans,2016: Progress and Opportunities in Reducing Racial Disparities. 2016: CA cancer J Clin 2016;66:290–308
Ref 3 National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Available at: https://seer.cancer.gov/statfacts/html/prost.html
Ref 4 Le Roux HA et al. Prostate Cancer at a regional hospital in South Africa: we are only seeing the tip of the iceberg. S Afr J Surg Vol. 53 no. 3&4. Dec 2015
Ref 5 Kirby RS, Patel M. Fast Facts: Prostate Cancer. Eight Edition 2014. Health Press Limited
Ref 6 Prostate Cancer UK. Are you at risk? Available at: https://prostatecanceruk.org/prostate-information/are-you-at-risk
Ref 7 Kicin´ski1 M, Vangronsveld J. An Epidemiological Reappraisal of the Familial Aggregation of Prostate Cancer: Available at: www.plosone.org Plos One. October 2011 | Volume 6 | Issue 10 | e27130
Ref 8 Lamy P. Trétarre B et al. Family history of breast cancer increases the risk of prostate cancer: results from the EPICAP study. Oncotarget, 2018, Vol. 9, (No. 34), pp: 23661-23669
Risk Factors for Prostate Cancer
(Compiled July 2018) (Revised January 2019)
The best known and proven risk factors for prostate cancer are advancing age, race and a positive family history of prostate cancer. There are other risk factors but there is less evidence for these.
Age
As men get older they are more likely to get prostate cancer. The risk for prostate cancer begins to rise sharply after age 55 years and peaks at age 70–74. Global statistics show that three quarters of prostate cancer occur in men over the age of 65 and that prostate cancer is rare in men below the age of 50. However it is important to note that black African men tend to get prostate cancer at a younger age. (See section on race and prostate cancer)
Race
In the USA the risk of prostate cancer is 60% higher in black American men compared to white males. The risk of dying of prostate cancer amongst Black African American men is also twice as high as that of white American men. The current statistics in South Africa are unreliable for a number of reasons but based on the studies from the USA and the UK we believe that black African men are at a much higher risk of getting prostate cancer than other race groups. The type of prostate cancer that they get is also is also likely to be more aggressive and to be passed on genetically.
Family history
There is strong evidence to show that a family history of prostate cancer increases a man’s risk of prostate cancer. Men who have a father or brother with prostate cancer are 2 to 3 times more likely to get prostate cancer themselves. The number of relatives with prostate cancer and their age at diagnosis is also important in terms of the likelihood of being affected at a younger age. Some studies show that having a mother or daughter who has had breast cancer also increases a man’s risk for prostate cancer.
References: Gann PH., Reviews in Urology. Vol 4, suppl. 5 2002
Other Modifiable Risk Factors for Prostate Cancer
Sexual Activity
There is strong evidence to suggest that men who have more frequent ejaculations (more than 21 a month), throughout their adult life are about 20% less likely to get prostate cancer. The ejaculations can be from sex, masturbation or nocturnal emissions.
Ref: Rider, Jennifer R. et al. Ejaculation Frequency and Risk of Prostate Cancer: Updated Results with an Additional Decade of Follow-up. European Urology , Volume 70 , Issue 6 , 974 – 982
Smoking
It is unclear whether smoking increases the risk for prostate cancer. However, there is data that shows that smokers have a 17% greater risk of dying from prostate cancer than non-smokers. Smoking greatly increases the risk of many other cancers so it’s worthwhile for men who smoke to quit.
Ref: Huncharek, Michael et al. Smoking as a Risk Factor for Prostate Cancer: A Meta-Analysis of 24 Prospective Cohort Studies. American Journal of Public Health 100.4 (2010): 693–701. PMC. Web. 20 June 2018.
Obesity
The relationship between obesity and prostate cancer is a complicated one. It is more difficult to detect prostate cancer in obese men for a number of reasons:
- They tend to have lower PSA scores
- They have larger prostates which mean that more cancers are likely to be missed when doctors perform a biopsy
- It is more difficult to perform a digital rectal examination on an obese man
All this means that prostate cancer is less likely to be detected in the early stages in obese men. Obesity is also associated with an increased risk for aggressive prostate cancer and a poorer outcome in men who are treated for prostate cancer. There is strong evidence linking obesity to a number of other serious diseases and for this reason we recommend that obese men get medical assistance to help them get there weight under control.
Ref: Allott, Emma H. et al. Obesity and Prostate Cancer: Weighing the Evidence. European Urology, Volume 63 , Issue 5 , 800 – 809
Dietary factors and prostate cancer
It is important to note that the evidence linking certain foods and vitamins to prostate cancer is not conclusive. We recommend that men follow a diet that has been proven to be good for overall health. Men should also be cautioned about the use of supplements to prevent prostate cancer as there is a possibility that some supplements could increase the risk. The following are some findings that will require additional research before the results can be considered conclusive and recommendations can be made. Please note that the evidence is not currently strong enough for these so we cannot make recommendations.
Saturated Fats
There is some evidence to show that the regular intake of saturated fats can increase the risk of prostate cancer. Saturated fats are animal fats found mostly mainly in dairy products and red meat.
Meat cooked at high temperatures
There is some evidence to show that eating meat that is well-done or meat that is cooked at a high temperature (e.g. grilled, fried, and barbecued meats) increases the risk for advanced prostate cancer. The more of this type of meat that is eaten the greater the risk.
Calcium
There is some evidence to show that a diet that is high in calcium increases the risk for prostate cancer.
Vegetables
A diet that includes plenty of fresh fruit and vegetables has strong health benefits and some of the components found in vegetables have antioxidant properties which may help to reduce the risk for cancer.
Lycopene
There is some evidence to show that lycopene can reduce the risk for prostate cancer through its antioxidant effect. Lycopene is a substance that is found in various foods. Foods containing high amounts of lycopene include cooked tomatoes and tomato based products like tomato sauce and tomato paste, guavas, watermelon, grapefruit, papaya, sweet red peppers, asparagus red cabbage and mangoes. However, to obtain significant levels of lycopene from tomatoes products like tomato paste are required as raw tomatoes have very low levels. To illustrate this, one slice of raw tomato contains 515 micrograms of lycopene whilst 2 tablespoons of tomato paste contains 13 800 micrograms. Cooking also alters the lycopene’s molecular structure so that it is more easily absorbed by the body.
Vitamin E
There is some evidence that taking a vitamin E supplement may increase the risk for prostate cancer.
References for Dietary Factors and Prostate Cancer
(1) Gathirua-Mwangi et al. Dietary factors and risk for advanced prostate cancer. European Journal of Cancer Prevention. 23(2):96–109, MAR 2014
(2) Ref: Ford N., Livestrong.com. Accessed on 30/06/2018. Available at: https://www.livestrong.com/article/344493-tomato-cooked-or-raw-lycopene/
(3) Ref: Gann PH. Risk factors for prostate cancer. Reviews in Urology. Vol 4, suppl. 5 2002.
(4) Klein EA et al. Vitamin E and the risk of prostate cancer: Updated results of the selenium and vitamin E cancer prevention trial (SELECT). JAMA. 2011 October 12; 306(14): 1549–1556. doi:10.1001/jama.2011.1437.
Alcohol and Prostate Cancer
There is strong evidence showing that alcohol increases the risk for mouth, throat, oesophageal, liver and colorectal cancer. (1) However the link between alcohol consumption and prostate cancer is less clear and studies have shown conflicting results. We cannot therefore make recommendations based on the current research.
Some evidence shows that men who are heavy regular drinkers and binge drinkers are at increased risk for prostate cancer whilst non-drinkers may be at increased of dying from prostate cancer compared to those who are light users of alcohol. (2)
Other studies show that alcohol consumption is not associated with overall prostate cancer risk or risk for low-grade prostate cancer but that the risk for high-grade prostate cancer is increased in men who consumed a minimum of seven drinks per week when aged 15 to 19 years compared with men who did not drink during that period of their lives. The same study showed that men with a higher cumulative alcohol intake throughout their lives were more likely to be diagnosed with high-grade prostate cancer. (3)
References for Alcohol and Prostate Cancer:
Ref (1) Testino G, Maedica. A Journal of Clinical Medicine, Volume 6 No.4 2011.
Ref (2) Dickerman A et al. Alcohol intake, drinking patterns, and prostate cancer risk and mortality: A 30-year prospective cohort study of Finnish twins. Cancer Causes Control. 2016 September ; 27(9): 1049–1058. doi:10.1007/s10552-016-0778-6.
Ref (3) Michael J, et. Cancer Prev Res. 2018; Early-Life Alcohol Intake and High-Grade Prostate Cancer: Results from an Equal-Access, Racially Diverse Biopsy Cohort. Available at http://cancerpreventionresearch.aacrjournals.org/content/early/2018/08/16/1940-6207.CAPR-18-0057
Symptoms of prostate cancer
(compiled June 2019)
There are generally no symptoms of prostate cancer in the early stages of the disease which is why screening is so important. Some of the symptoms of prostate cancer are the same as the symptoms for an enlarged prostate (benign prostatic hyperplasia or BPH). This condition is also common in older men.
Symptoms in Early (localised) Prostate Cancer
Localised prostate cancer is when the cancer is contained within the prostate. There are generally no symptoms at this stage which is why screening is so important.
Symptoms for locally Advanced Prostate Cancer
At this stage the cancer tumour may have spread to areas surrounding the prostate such as the bladder, the pelvic nerves, the urethra and the seminal vesicles. The tubes carrying the urine (ureters) can be blocked. The following symptoms can occur:
- A need to urinate frequently, especially at night
- An urgent need to urinate
- Difficulty starting urination or holding it in
- Weak or interrupted flow of urine
- Painful urination
- Blood in the urine or semen
- Erectile dysfunction
- Loin pain
- Very little or no urine
- When the tumour enlarges it can push against the rectum which sits behind the prostate causing constipation, cramping and rectal bleeding.
Symptoms for Advanced Prostate Cancer (Metastatic Prostate Cancer)
When prostate cancer spreads to other body parts it may cause:
- Bone pain particularly in the pelvis and lower spine due to bone metastases (cancer tumours that develop in the bones)
- Bone fractures
- Spinal cord compression causing a loss of feeling in the limbs
- Lymph node enlargements
- Loin pain due to a blockage in the tubes carrying urine from the kidneys to the bladder
Other symptoms that occur when the cancer is spread widely throughout the body can include:
- Lack of energy from iron loss (anaemia)
- Weight loss with muscle wasting and loss of appetite
References 1 – Kirby RS, Patel M. Fast Facts: Prostate Cancer. Eight Edition 2014. Health Press Limited
Screening for prostate cancer
(Updated 25 June 2024)
What screening tests are recommended?
For men who are not experiencing any symptoms, a Prostate Specific Antigen (PSA) blood test is the recommended first line test. The rapid PSA test is not recommended as a screening test for prostate cancer as it does not use age related reference ranges.
Before deciding on whether to go for prostate cancer screening you should understand the following:
- Disadvantages of screening
The PSA blood test is not a cancer specific test. In about 75 out of 100 cases when the PSA is raised there is no prostate cancer which means that something other than cancer has caused it to be higher than normal (false positive). This may cause unnecessary anxiety in men. An enlarged prostate is often the cause of a slightly higher than normal PSA score.
– In about 15 out of every 100 men who have a normal PSA there is prostate cancer (false-negative result). This may cause men who have had a PSA to believe that they are cancer free when in fact they have prostate cancer.
– The PSA test may detect a type of prostate cancer that is slow-growing and non-aggressive and that may never cause a problem. Men with this type of prostate cancer who opt for active treatment may be worse off because of the side effects of treatment which negatively affect their quality of life. However, “active surveillance” can avoid over-treatment in men with low risk for disease progression. - Advantages of screening
– Men who don’t go for screening could end up with prostate cancer that has spread (metastatic prostate cancer) and which can never be cured. The treatments for metastatic prostate cancer have a major impact on a man’s quality of life as they involve removing testosterone (the male hormone) from the body.
– Screening can help detect prostate cancer in the early stages when it can be cured. Early detection of prostate cancer reduces the risk of dying from prostate cancer by up to 56%.
– Screening can reduce anxiety if the screening results are negative.
At what age should South African men consider going for screening?
Informed patient-based screening is recommended in men with a life expectancy of more than 10 years in the following situations:
– From the age of 40 in black African men and in men who have a family history of prostate and/or breast cancer in a first degree relative.
– From the age of 45 years for all other men
– In men who have undergone genetic testing and who are carriers of prostate cancer risk germline mutations, screening should be done at age 40 or at 10 years younger than the age of onset of the youngest affected family member if this is before 40
Germline mutations that increase the risk for prostate cancer include: BRCA2, BRCA 1, HOXB13, ATM, CHEK2, PALB2, MLH1, MSH2, MSH6, PMS2, EPCAM and TP53 genes.
In addition, patients with a history of lower urinary tract symptoms (LUTS) and/or clinical suspicion of prostate cancer, regardless of age group, should have their PSA tested.
Recommended screening intervals
Men with a low initial PSA level (PSA ≤1.0 ng/mL) can screen every two years and those with higher levels should screen annually.
Due to their increased risk for PCa, Black African men should consider screening annually.
Men with a mutation in a PCa-associated gene, or a strong family history of PCa should screen annually.
The Prostate Specific Antigen (PSA) test
Prostate specific antigen is a type of protein that enters the blood when the barriers in the prostate are damaged. It is a simple blood test that gives an indication of whether something is wrong with your prostate. It is not a cancer specific test. A high PSA test result could be caused by:
– an enlarged prostate
– an infection/inflammation of the prostate (prostatitis)
– prostate cancer
Avoid the following activities for 48 hours before a PSA test:
– cycling
– ejaculation
Your PSA result may not be accurate:
- if you have an active urinary tract infection
- after recent urinary tract instrumentation and/or urinary retention
- if you have had a prostate biopsy in the previous 6 weeks
- if you are taking medication such a finasteride or dutasteride for an enlarged prostate or hair loss (5-alpha reductase inhibitor)
Normal PSA Scores
The most common threshold used to define a high PSA is ≥4 ng/mL. The use of age-related references improves detection rates and it is therefore recommended rather than using the traditional threshold of 4 ng/mL.
• 40 – 50 years 0 – 2.5 ng/mL
• 50 – 60 years 0 – 3.5 ng/mL
• >60 years 0 – 4.0 ng/mL
Chances of having prostate cancer diagnosed for a PSA ≥4.0 ng/mL is approximately 25%
Chances of having prostate cancer diagnosed for a PSA ≥10 ng/mL is approximately 60%
Measuring Free PSA
This is a variation of the normal PSA test that is used to distinguish between men who have an enlarged prostate as opposed to prostate cancer. It measures PSA that is not bound to protein in the serum.
PSA Velocity
If you have been having regular PSA tests over 1 to 2 years and there are more than 3 test results available your doctor may also check to see how much the PSA score has changed over time and how quickly it has risen. If the PSA changes by more than 0.75ng/ml in a year, this can give an indication of potential prostate cancer even though the score is still within the normal range.
The Digital Rectal Examination (DRE)
The digital rectal examination is no longer considered necessary to screen for prostate cancer in men who are not experiencing symptoms, and who have a PSA that falls within the normal range for their age.
What happens if your PSA is high ?
If your PSA is high it will often be retested. If it is still high you will generally be referred to a urologist for further investigation.
The urologist will perform a full assessment to determine the reason for the raised PSA.
This will include a digital rectal A lot of men are embarrassed about this test but it is quick and there are only a few seconds of minor discomfort. The examining doctor inserts a gloved and lubricated finger into the rectum so that they can feel the prostate for any abnormal lumps, hardening, asymmetry or a lack of mobility.
If your urologist suspects prostate cancer you may be referred for a special type of MRI scan called a multiparametric MRI scan.
A prostate biopsy is used to diagnose prostate cancer. A biopsy involves inserting a number of needles into the prostate in order to obtain a small sample of the prostate cells which are then sent to a laboratory to be checked for cancer.
References
(1) Advising men aged 50 and over about the PSA test for prostate cancer: information for GPs. Available at: https://www.gov.uk/government/publications/prostate-specific-antigen-testing-explanation-and-implementation Last accessed on 5 October 2019.
(2) Kirby RS, Patel I. Fast Facts: Prostate Cancer. Eighth edition. Health Press Limited. Jan 2014
(3) Hoffman RM. Screening for prostate cancer. Available on: https://www.uptodate.com/contents/screening-for-prostate-cancer Last accessed 24 July 2019
(4) South African Prostate Cancer Guidelines June 2024
Prostate Biopsy and Magnetic Resonance Imaging
Updated on 25 June 2024
If your PSA test is high, or your doctor felt anything abnormal when doing a digital rectal examination, or you have other signs and symptoms of prostate cancer you will be referred to a urologist for further examination. The urologist will take a thorough history. It is important to advise your urologist of any family history of prostate, breast and other cancers. A digital rectal examination will be performed to feel for any signs of prostate cancer.
Your urologist may do a number of other tests to decide whether a prostate biopsy is necessary.
Multiparametric Magnetic Resonance Imaging (mp-MRI) (1) (2) (3)
Since its introduction, this technology has made a huge difference to the field of prostate cancer diagnosis. It is recommended that an mpMRI is performed before a biopsy. Magnetic resonance imaging (MRI) uses a strong magnetic field, radio waves, and special computer software to show detailed images of the prostate and anything unusual in it, or around it. The size, shape and location of tumours can be identified, which assists with staging and gives an indication of how aggressive the cancer is. MRI also has the advantage of being non-invasive and there is no exposure to radiation. It is done at a radiology facility and the results are interpreted by a radiologist. An MRI also helps the urologist to identify areas that need to be targeted for the biopsy. Up to four different parameters may be used to check for cancer cells when doing a prostate MRI.
Parameter 1 – T2 weighted MRI (T2 MRI)
This gives a 3D map of prostate zone anatomy and identifies suspicious looking areas.
Parameter 2 – Diffusion weighted imaging (DWI MRI)
This shows the movement of water molecules in tissue which helps to identify cancer cells which restrict the motion of water
Parameter 3 – Dynamic contrast enhanced imaging (DCE MRI)
Here a contrast agent is injected into a vein and it shows the blood flow in the tumour which is different to blood flow in normal tissue.
Spectroscopy (MRI-S) may be added as a fourth parameter.
This procedure identifies cancer cells by the chemical metabolites that they produce which are different from normal cells.
A Prostate Biopsy
This is the procedure that is used to diagnose prostate cancer. It involves extracting tissue samples from the prostate using special thin hollow biopsy needles. A prostate biopsy is usually done using an ultrasound probe inserted in the rectum which provides a live image of the prostate. This enables the urologist to see where the biopsy needles are being inserted, so that samples of tissue can be taken from different areas within the prostate. The samples are then sent to a pathology laboratory where the cells from each needle (core) are examined and graded according to how badly the cancer has affected the tissue. This grading is called a Gleason score is covered in the section “Understanding Your Laboratory Results from a Prostate biopsy.” This is called a histological diagnosis. It’s important to understand that no biopsy is 100% reliable as the needles may miss the tumour, particularly if it is very small or if the prostate is large.
Types of prostate biopsies
Random Systematic 12-core sextant biopsy (SBx)
In this procedure transrectal ultrasound (TRUS) imaging is used to visualize the prostate gland. This involves inserting an ultrasound probe up the rectum which then provides a live image of the prostate and helps the urologist to guide the biopsy needles into different parts of the prostate. Normally 12 to 14 needles (referred to as cores) are then inserted systematically into different parts of the prostate. With this method about one third of clinically significant prostate cancers will be missed. In men who have large prostates the percentage of prostate tissue that is sampled is naturally lower and the results are therefore less reliable.
MRI Targeted Biopsies
A greater number of prostate cancers can be diagnosed through the MRI targeted biopsy procedure and this therefore the recommended option when available. They also help urologists to detect more of the problematic prostate cancers (clinically significant cancers that are likely to progress) and less of the non-problematic cancers.
A Cognitive Prostate Biopsy
This has become the preferred method for many urologists who routinely do an MRI before the biopsy as it does not require any additional equipment. If you have had an MRI before the biopsy then the urologist will review the MRI images before and during the biopsy and use the information to guide where best to take samples from within the prostate. The success of this technique is very much dependent on the urologist’s ability to translate MRI images to transrectal ultrasound without a physical overlay of the two images (operator dependant). Cognitive fusion biopsies have a higher detection rate than random biopsies.
MRI/TRUS Fusion Guided Biopsy
New technology is now available to combine or “fuse” MRI images with the live imaging from transrectal ultrasound. This MRI/TRUS fusion technology involves the use of sophisticated software to combine the two images. Remember that the MRI provides a clear image of where the “area of interest” in the prostate is, so with this technology the urologist can guide the biopsy needles directly to the potential tumour. This means that fewer needles will need to be used. This technology is still very new in South Africa and urologists that use this technique require additional training, but the results are less “operator dependant” than a cognitive biopsy. This biopsy method is particularly useful for patients who continue to have a high PSA or suspicious DRE but who have a negative biopsy result using the random biopsy method.
There are two routes that urologists use for performing a biopsy:
Transperineal biopsy
In a transperineal biopsy, the needles are inserted through the perineum (the area between the scrotum & the anus) after a small cut is made. There is less risk of infection with this procedure compared to a transrectal biopsy and it is therefore the recommended biopsy method. The procedure is however more painful than a transrectal biopsy.
Transrectal biopsy
In a transrectal biopsy the needles are inserted through the rectum. There is a higher risk of infection from transrectal biopsies as bacteria from the rectum can be transferred via the biopsy needle to the urinary tract, blood circulation and the prostate. There is also a higher risk of bleeding.
Some urologists require their patients to use an enema to empty the bowels of all faeces before the procedure. An antibiotic is always used to help prevent infections. It’s important to tell your doctor if you are taking any medications that can increase the risk of bleeding such as; warfarin, aspirin, ibuprofen or any other type of anticoagulant including natural herbal products. Your doctor will advise you when to stop taking these medications to prevent excessive bleeding from the procedure.
Anaesthetic
The procedure may be performed under general anaesthetic or whilst you are awake using local anaesthetic.
After the procedure
You may have some pain and bleeding from your rectum if you had a transrectal biopsy or from the perineal area if you had a transperineal biopsy.
There may be blood in your urine, stools and semen for a few days after the procedure. See your doctor if you experience any of the following symptoms:
- a fever
- difficulty urinating
- prolonged or heavy bleeding
- increasing pain
References
Ref 1 – Kirby RS, Patel M. Fast Facts: Prostate Cancer. Eight Edition 2014. Health Press Limited
Ref 2 – De Visschere PJ, Briganti A, Fütterer JJ, et al. Role of multiparametric magnetic resonance imaging in early detection of prostate cancer. Insights Imaging. 2016;7(2):205-14.
Ref 3 – Brown EM et al. Recent advances in image-guided targeted prostate biopsy. Abdom Imaging. 2015 August ; 40(6): 1788–1799
Ref 4 – Andrea B et al. The Role of MRI-TRUS Fusion Biopsy in the Diagnosis of Clinical Significant Prostate Cancer (CsPca)
Ref 5 – Xiang J. Transperineal versus transrectal prostate biopsy in the diagnosis of prostate cancer:
a systematic review and meta-analysis. World Journal of Surgical Oncology (2019) 17:31
Understanding Your Biopsy Results and Gleason Score
Compiled 20 Jan 2020
Your pathology laboratory report after a prostate biopsy will provide key information as to how aggressive the cancer is. Understanding your results will help you to make an informed decision about the treatment options available to you.
Your laboratory results will include a Gleason score which is one of the most important indicators of how aggressive the prostate cancer is and what treatment options will be suitable. 1However, it needs to be interpreted together with your other test results. Always get a copy of your laboratory report as it contains critical information that you will need if you wish to get a second opinion or if you want to do any research of your own about your diagnosis. You need to be aware that it is possible that a negative biopsy report doesn’t rule out the possibility that you may have prostate cancer.1
Each needle (core) obtained from a biopsy is analysed separately and the pattern of the tissue in each core is given a separate diagnosis. 2The pathologist assigns a grade between 1 and 5 to each sample. A grade 1 pattern when viewed under a microscope looks most like normal tissue and a grade 5 pattern is the worst as the tissue appearance is very abnormal. 2 Although grades 1 and 2 appear different, they are now reported as a grade 3 as they have the same outcomes. A pure grade 3 cancer is unlikely to ever metastasize.3
The overall number of cores (biopsy needles) that are positive for cancer and the percentage of each core that is made up of cancer, gives an indication of the tumour size.
How is a Gleason Score Calculated?
The Gleason score is most often obtained by adding the number of the most common Gleason pattern with the second most common. The lower the score the less aggressive the cancer and the less likely it is to progress. The exception to this is if any one of the cores contains a lot of high-grade cancer, or there are 3 grades that include high-grade cancer. In these two instances the Gleason score is modified to show the aggressive nature of the cancer so that the most suitable treatment options can be selected.2 Gleason scores of 1 and 2 are now reported as a Gleason 3 as cancer with these patterns has an outcome no different from grade 3. 3
It is important when interpreting a Gleason score to understand that the order of the numbers is highly significant as the first number is always the most prevalent type of pattern found. So even if the total is 7, a Gleason score of 4 + 3 = 7 is worse than a Gleason score of 3 + 4 = 7. That’s because 4 indicates a more aggressive cancer so if it is the most prominent in all of the cores, that’s worse than if 3 was the most prominent. 2
What do different Gleason scores mean?
If there are multiple cores with different grades they will be reported separately and ideally by anatomical site.3Prostate cancer can have areas with different grades. To get a total Gleason score the pathologist will use the grades from the 2 areas that make up most of the cancer. 2
Gleason 6– Is considered low grade. The lowest score from cancer found on a biopsy is 6. These cancers are most often non-aggressive and slow growing.2Many insurance companies will not pay out for dread disease cover for a Gleason 6 score.
Gleason 7 is considered intermediate risk but there is a difference:1
Gleason 3+4 = 7 Cancers with this grade still have a good outlook (prognosis), but not as good as a Gleason 6
Gleason 4+3 = 7 Cancers with this grade are more likely to grow and spread than a 3+4=7
but not as much as a Gleason 82 1
Gleason 8 – This is considered a high grade cancer1
Gleason 9 to 10 These are also high grade cancers but are twice as likely as a Gleason 8 to grow and spread quickly 2
A new system has now been developed which makes it a lot easier to understand the Gleason score and how high risk the prostate cancer is. The Gleason scores are reported in Grade Groups as per the table below.2
International Society of Urological Pathology 2014 grade (group) system
| Gleason score | ISUP grade |
| 2-6 | 1 |
| 7 (3+4) | 2 |
| 7 (4+3) | 3 |
| 8 (4+4 or 3+5 or 5+3) | 4 |
| 9-10 (4+5 or 5+4 or 5+5) | 5 |
Some of the other things that may be reported on your pathology report:
Adenocarcinoma
This is the most common type of cancer found in the glandular cells of the prostate
Perineural invasion2
This means cancer was seen alongside a nerve fibre within the prostate and that the cancer has possibly spread outside of the prostate.
Prostatic Intraepithelial Neoplasia (PIN) and Atypical Small Acinar Proliferation (ASAP 1 2
PIN indicates that there are irregular abnormal cells. Although they are not currently cancerous, high grade PIN is very similar to cancer cells and can be an indication that cancer may be present in other parts of the prostate.
Acute inflammation (acute prostatitis) or chronic inflammation (chronic prostatitis)2
Prostatitis is inflammation of the prostate. It doesn’t affect the cancer diagnosis
Atrophy, adenosis or atypical adenomatous hyperplasia?2
These are types of conditions of the tissues that can be seen by the pathologist when examining the biopsy samples. They are non-cancerous.
Seminal vesicle2
This is another gland, that like the prostate, makes up part of the seminal fluid. There are two that are situated just behind the prostate and when prostate cancer spreads it is often to one or both of the seminal vesicles. Sometimes, a biopsy sample will have been taken from the seminal vesicles.
Atypical glands, atypical small acinar proliferation (ASAP), glandular atypia, or atypical glandular proliferation2
These are patterns that could potentially be cancer but are not clear enough to be graded.
References:
Ref 1 – TRUS and biopsy results. Prostate Cancer UK. Available at: https://prostatecanceruk.org/for-health-professionals/online-learning
Ref 2 – Understanding Your Pathology Report: Prostate Cancer. Association of Directors of Anatomic and Surgical Pathology. American Cancer Society. Last reviewed March 2017. Available at: https://www.cancer.org/treatment/understanding-your-diagnosis/tests/understanding-your-pathology-report/prostate-pathology/prostate-cancer-pathology.html
Ref 3 – Iczkowski K. Grading (Gleason). PathologyOutlines.com, Inc. Available at: http://www.pathologyoutlines.com/topic/prostategrading.html Updated June 2016
Tests to detect if prostate cancer has spread
Compiled April 2020
If your doctor suspects that the prostate cancer has spread to other parts of your body you may be referred for additional tests. Once prostate cancer spreads out of the prostate it spreads to surrounding tissues and structures. The cancer cells can then enter the blood and lymph vessels and spread throughout the body to bone and soft tissue, where they re-implant and grow to form secondary tumours or metastases. These metastases are still made up of prostate cancer cells.
It is important for your doctor to know whether the prostate cancer has spread outside of the prostate and if so where. This helps with staging and planning the treatment.
If the cancer recurs after treatment, imaging tests may be required to determine where the cancer has spread to in order to plan further treatment.
Some tests are better than others at finding metastases in different tissues which is why your doctor may order more than one type of test. Not all tests may be available at all facilities and some tests are very expensive. No test is 100% accurate and initially the cancer cells that spread might be very small (micro metastases) and therefore undetectable by some tests.
Most tests will be done at a radiology/nuclear medicine facility. The test results will be analysed by a radiologist/nuclear physician (a medical doctor who specialises in the diagnosis of diseases and injuries using medical imaging). The tests are normally done by a radiographer who works under the supervision of a radiologist. Some tests require that you have an injection with a radioactive dye. It’s important to tell the healthcare workers if you have any allergies.
Tests to detect if cancer has spread to lymph nodes
Prostate cancer tends to spread first to regional lymph nodes in the pelvic area. Lymph nodes are part of the lymphatic system. The lymphatic system consists of lymph vessels and lymph nodes and is part of the body’s immune system. The lymph vessels carry lymph fluid, which contains nutrients and other substances, to the body’s tissue cells. Lymph vessels also remove and transport damaged cells, cancer cells, bacteria and viruses from tissues. These are then filtered out when the lymph fluid travels through the lymph nodes which are like filters. The cancer cells can also grow inside the lymph nodes. The following test may be used to determine if any lymph nodes have been affected.
CT
MRI
PET -CT/MRI (PSMA, Choline)
SPECT-CT (Tc-99m PSMA)
Tests to detect if cancer has spread to bone (bone metastases)
Prostate cancer commonly spreads to bones. It will often first spread to the bones in the pelvis and lower spine. The cancer can affect bones by activating cells in the bone resulting in abnormal bone production. This results in abnormal build-up of bone and the formation of osteoblastic lesions. The cancer can also cause abnormal destruction of bone causing osteolytic lesions. This is important because tests that are good at detecting osteoblastic lesions may not be good at finding osteolytic lesions. Some patients may have a mixture of both types of lesions. The following tests may be used to check for bone metastases:
Standard X-rays
Bone scan (this test is increasingly being replaced by newer tests that are far more accurate)
Especially when prostate cancer recurs or PSA is low – PET/CT or MRI
For patients who have undergone a radical prostatectomy – PSMA PET/CT or SPECT-CT
Tests used to detect if cancer has spread to soft tissue other than lymph nodes (visceral metastases)
Prostate cancer can also spread to organs like the liver, digestive system, kidneys, adrenal glands and brain. These are called visceral metastases. Tests use to check if prostate cancer has spread to organs can include.
PET-CT/MRI
SPECT/CT (PSMA)
Whole body MRI (with diffusion-weighted imaging WB-MRI)
| Summary of Types of Tests used to check if prostate cancer has spread (metastasized) | What the Test Shows |
| X-Rays of the lower back and pelvis | Abnormal (hard)whitening of the tissue on bone (sclerotic metastases) or more rarely decreased whitening (osteolytic metastases) |
| Bone Scans
This is an older test with limited value particularly in men with a PSA <20 |
Bone scans show if the cancer has spread to the bones (bony metastases). |
| SPECT-CT | This is similar to a bone scan but provides a 3D image and can show lesions smaller than 1cm. It is more accurate than a traditional bone scan |
| CT (computed tomography)
PET CT/MRI (positron emission tomography /in combination withcomputed tomography /magnetic resonance imaging MRI Scans (magnetic resonance imaging) |
These scans show a slices through the body and can show cancer tumours (metastases), that have spread to different parts of the such as bone, lymph nodes, the liver and other organs
Whole body MRI may be more accurate than a bone or CT scan for identifying and measuring bony metastases |
| (PMSA) PET CT /MRI Scan prostate-specific membrane antigen positron emission tomography/computed tomography scan | This test may be the most sensitive compared to other imaging modalities as it has been shown to be able to identify metastases in patients even with very low PSA levels (most commonly used to detect if cancer cells have returned after treatment. It can detect lesions even if the PSA score is <0.5 ng/ml. |
| (T99m PMSA) SPECT/CT prostate-specific membrane antigen positron emission tomography/computed tomography scan | This test is similar to PSMA PET/CT but slightly less sensitive |
- Coetzee L. Metastatic Prostate Cancer. Health Press Limited 2017.2. Turpin A et al. Imaging for Metastasis in Prostate Cancer: A Review of the Literature. Front. Oncol. 10:55. doi: 10.3389/fonc.2020.00055. Available at www.frontiersin.org.
- Turpin A, (2020) Imaging for Metastasis in Prostate Cancer: A Review of the Literature. Front. Oncol. 10:55. doi: 10.3389/fonc.2020.00055
- Tabotta et al. BMC Musculoskeletal Disorders (2019) 20:619. Available at: https://doi.org/10.1186/s12891-019-3001-6
- Futterer JJ et al. Imaging modalities in synchronous oligometastatic prostate cancer. World Journal of Urology 2018. Available at: https://doi.org/10.1007/s00345-018-2416-2
- Lengana T et al. Ga-PSMA PET/CT Replacing Bone Scan in the Initial Staging of Skeletal Metastasis in Prostate Cancer: A Fait Accompli? Clin Genitourin Cancer. 2018 Oct;16(5):392-401. doi: 10.1016/j.clgc.2018.07.009.
- Hofman MS et al . proPSMA Study Group Collaborators. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. Lancet. 2020 Apr 11;395(10231):1208-1216. doi: 10.1016/S0140-6736(20)30314-7.
- Giesel FL et al. Detection Efficacy of (18)F-PSMA-1007 PET/CT in 251 Patients with Biochemical Recurrence of Prostate Cancer After Radical Prostatectomy. J Nucl Med. 2019 Mar;60(3):362-368. doi: 10.2967/jnumed.118.212233. Epub 2018 Jul 24. PubMed PMID: 30042163
Prostate Cancer Stage and Grade
It is important for your doctor to have an indication of the stage of your prostate cancer as this determines what treatment options are available to you.
Clinical staging
This is done before treatment is initiated and is based on the results of your digital rectal exam (DRE), your PSA score, Gleason grading and biopsy results. If any other investigations like an MRI, X-Rays, bone scans, CT and PET scans have been done, these will also help with staging.
Pathologic staging
If you have surgery to remove the prostate (a radical prostatectomy) your cancer will be restaged. This sentence doesn’tlead on logically from the one before -This is because the prostate and surrounding tissue removed during surgery including any affected lymph nodes are sent to a laboratory for analysis. This is more accurate than clinical staging. Pathologic staging is indicated by a ‘p’.
The laboratory report will also indicate whether the surgical margins were positive. The surgical margin is the edge of the tissue surrounding the removed tumour. Ideally,these should be free of any cancer cells (a negative margin). A positive surgical margin means that cancer cells were found by the pathologist at the edge of the removed tumour which could mean that not all of the cancerous tissue was removed.
The most common method to stage prostate cancer is the TNM method.
The information below is adapted from the AJCC Cancer Staging Handbook from the American Joint Committee on Cancer.
T – indicates the tumour size and how far it has spread
N – describes lymph node involvement
M – indicates whether or not the cancer has spread (metastasised) to bones or other organs
T- Tumour Staging (Clinical staging)
Stage T1
This is the earliest stage of prostate cancer and the cancer is usually slow growing
The tumour cannot be felt on DRE and it is not visible with imaging tests
PSA levels are usually low
T1a8
The tumour is usually found when prostate tissue is examined for other reasons (for example removal of prostate tissue due to an enlarged prostate)
Only 5% of the tissue sample examined has cancer
T1b8
The tumour is usually found when prostate tissue is examined for other reasons
The cancer is found in more than 5% of the tissue sample examined
T1c8
The tumour is identified by a needle biopsy which is done because of a raised PSA
Stage T2
There is increasing risk of the cancer growing and spreading
The cancer has not spread out of the prostate
PSA levels are usually low or medium
T2a
The tumour involves half of one lobe or less
The tumour cannot be felt on DRE
T2b
The tumour involves more than one half of one lobe but not both lobes
The tumour may be large enough to be felt on DRE
T2c
The tumour involves both lobes
The tumour may be large enough to be felt on DRE
Stage T3
The tumour has spread outside of the prostate capsule
The tumour is growing or the cancer is high grade
PSA levels are usually high
These are all indications of a locally advanced cancer that is likely to grow and spread
T3a
Tumour has spread outside of the prostate capsule on one or both sides
T3b
Tumour has spread outside of the prostate and invades one or both seminal vesicles
Stage T4
The tumour is fixed. 8This means that cancer cells have spread from the initial tumour in the prostate and haveattached to other tissue completely different from the prostate – normally the pelvic wall.
Or
the cancer invades structures outside of the prostate (other than the seminal vesicles) such as the; external sphincter, rectum, bladder, levator muscles and/or the pelvic wall.8
N-Staging (involvement of lymph nodes)
The lymphatic system consists of lymph vessels and lymph nodes and is part of the body’s immune system. The lymph vessels carry lymph fluid, which contains nutrients and other substances, to the body’s tissue cells. Lymph vessels also remove and transport damaged cells, cancer cells, bacteria and viruses from tissues. These are then filtered out when the lymph fluid travels through the lymph nodes which are like filters. The cancer cells can also grow inside the lymph nodes.
When cancer spreads (metastasizes) it is often first to the lymph nodes around the prostate. The cancer can also spread to lymph nodes further away from the prostate (distant lymph nodes), in which case the cancer is classified as metastatic prostate cancer.
The involvement of lymph nodes is an important part of the staging and is indicated by the letter ‘N’. If the distant lymph nodes are affected this will be indicated under the metastatic cancer classification (M).
N0
No regional lymph nodes affected by cancer
N1
The cancer has spread (metastasized) to the regional lymph nodes
M stage (Distant metastases)
The M staging describes whether or not the cancer has spread to other parts of the body not near the prostate and to what types of tissue it has spread eg lymph nodes, bone or soft tissue organs like the liver and lungs .
M0
No distant metastases (there is no evidence that the cancer has spread)
M1 –There is evidence of distant metastases
M1a –There is evidence that the cancer has spread to nonregional lymph nodes
M1b –There is evidence that the cancer has spread to bone(s)
M1c –The cancer has spread to other sites with or without bone disease
The different stages of prostate cancer
Localised Prostate Cancer
Prostate cancer that is still contained within the prostate is classified as localised prostate cancer. However, localised prostate cancer is further classified into different risk categories based on factors such as PSA levels, the Gleason score and the tumour grade. This is important, as the treatment options available may differ depending on the risk stratification. Different professional societies use different risk stratifications.
EAU Risk Stratification for biochemical recurrence of clinically localised prostate cancer based on the Gleason score and tumour stage assessed by digital rectal examination.
| Low-risk | Intermediate-risk | High-risk | ||
| Favourable | Unfavourable | |||
| ISUP grade 1 and
PSA < 10 ng/mL and cT1-2a* |
ISUP grade 2 and
PSA<10 ng/ml and cT1-2b* Or ISUP grade 1 and PSA 10– 20 ng/ml and cT1-2b* Or ISUP grade 1 and PSA <10 ng/ml and cT2b* |
ISUP grade 2 and
PSA10 – 20 ng/ml and cT1-2b* Or ISUP grade 3 and cT1-2b* |
ISUP grade 4/5
Or PSA > 20 ng/ml Or cT2c* |
cT3-4* and/or
cN+** any ISUP grade* any PSA |
| Localised prostate cancer | Locally advanced
prostate cancer |
|||
Ref: EAU Guidelines. Edn. presented at the EAU Annual Congress Milan 2023. ISBN 978-94-92671-19-6.
Available at: https://uroweb.org/guidelines/prostate-cancer/summary-of-changes/2023
The NNC provides a more detailed classification of risk groups
| Risk Group | Clinical/Pathologic Features | ||
| Very low | Has all of the following:
• cT1c • Grade Group 1 • PSA <10 ng/mL • Fewer than 3 prostate biopsy fragments/cores positive, ≤50% cancer in each fragment/corea • PSA density <0.15 ng/mL/g |
||
| Lowf | Has all of the following but does not qualify for very low risk:
• cT1–cT2a • Grade Group 1 • PSA <10 ng/mL |
||
| Intermediatef | Has all of the following:
• No high-risk group features • No very-high-risk group features • Has one or more intermediate risk factors (IRFs): ► cT2b–cT2c ► Grade Group 2 or 3 ► PSA 10–20 ng/mL |
Favourable intermediate | Has all of the following:
• 1 IRF • Grade Group 1 or 2 • <50% biopsy cores positive (eg, <6 of 12 cores)a |
| Unfavourable intermediate | Has one or more of the following:
• 2 or 3 IRFs • Grade Group 3 • ≥ 50% biopsy cores positive (eg, ≥ 6 of 12 cores)a |
||
| High | Has no very-high-risk features and has exactly one high-risk feature:
• cT3a OR • Grade Group 4 or Grade Group 5 OR • PSA >20 ng/mL |
||
| Very high | Has at least one of the following:
• cT3b–cT4 • Primary Gleason pattern 5 • 2 or 3 high-risk features • >4 cores with Grade Group 4 or 5 |
||
Ref: NCCN Clinical Practice Guidelines in Oncology. Prostate Cancer. Version 4.2023 — September 7, 2023.
Biochemical Recurrence ( A rising PSA after treatment of localised prostate cancer)
Men who have been treated for localsised prostate cancer with radiotherapy (brachytherapy or external beam radiation) or who have had a radical prostatectomy will have to go for regular PSA tests. A rising PSA level can happen months or many years after treatment and is usually the first indicator that the cancer may be recurring. If imaging test show no signs of the cancer spreading then this is referred to as biochemical recurrence. Biochemical recurrence may precede imaging findings or symptoms of active disease by months or even years.
The PSA levels that define recurrence are determined by the type of treatment a patient has previously received.
Biochemical recurrence after a radical prostatectomy
In patients who have had a prostatectomy, the PSA levels should fall to undetectable levels ie. below 0.1ng/ml.
This is called PSA nadir or the lowest level of PSA. If the PSA levels increase and reach a level of 0.2 ng/ml or more on two consecutive occasions then this is regarded as recurrent disease.
Biochemical recurrence after radiation therapy
Monitoring PSA levels in patients after radiation therapy is more complicated as the PSA doesn’t reach undetectable levels as with
surgery, because some prostate tissue remains. PSA levels decline gradually after treatment and it can take 18 months or even longer for the PSA to reach the lowest levels (PSA nadir). In patients who have had external beam radiation or brachytherapy, a PSA rise of 2ng/ml above nadir (the lowest PSA level reached after therapy) is indicative of recurrence.
Cancer progression after biochemical recurrence
Biochemical recurrence doesn’t necessarily predict the development of metastases. Several other factors affect how quickly the cancer is likely to progress as well as the type of treatment that may help
Metastatic Prostate Cancer
Prostate cancer is classified as advanced or metastatic if:
The cancer has spread to non-regional lymph nodes
and/or the cancer has spread to bone
and/or the cancer has spread to other sites with or without bone disease.
There is no cure for metastatic prostate cancer, however there are an ever increasing number of treatments that can help slow the progression of the disease and even delay the onset of symptoms caused by the cancer.
The number and location of the metastases will have an impact on how long patients are likely to survive. Patients with only bone metastases tend to live longer than patients with visceral metastases (cancer that has spread to organs such as the liver, kidneys etc).
Lower risk metastatic prostate cancer (oligometastatic prostate cancer)
This is a relatively new definition which describes a prostate cancer that is between localised and widespread metastatic prostate cancer. It means that the cancer has not spread widely. There is no agreement on the number of sites that it has spread to and definitions vary between 3 and 5 metastatic sites that affect only bone and or lymph nodes. The cancer appears to be more slow growing than the usual metastatic prostate cancer. Treatment is aimed at the sites of the mettases.
References:
- Prostate Cancer: Stages and Grades. Cancer.Net Editorial Board, 11/2019. Available at: https://www.cancer.net/cancer-types/prostate-cancer/stages-and-grades
- AJCC Cancer Staging Manual. Seventh Edition 2010. America Joint Committee on Cancer. Springer.
- Coetzee L. Metastatic Prostate Cancer. Health Press Limited 2017.
- Klaassen Z. The Impact of Visceral Metastasis in Prostate Cancer Patients. Urotoday. Available at: https://www.urotoday.com/library-resources/mcrpc-treatment/111525-the-impact-of-visceral-metastasis-in-prostate-cancer-patients
- Oligometastatic Prostate Cancer: A Shrinking Subset or an Opportunity for Cure? Rao et al. American Society of Clinical Oncology 2019.
- Muambirwa S. Understanding Recurrent and Metastatic Prostate Cancer. Feb 2022. MedEd/Ronin-Do (Pty) Ltd.
- EAU Guidelines. Edn. presented at the EAU Annual Congress Milan 2023. ISBN 978-94-92671-19-6. Available at: https://uroweb.org/guidelines/prostate-cancer/summary-of-changes/2023
- Schaeffer EM, Scrinvas S, Adra N, et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines). Prostate Cancer. Version 4.2023 – 7 September. 2023.
A prostate cancer diagnosis – what now?
Updated 25 June 2024
Being diagnosed with prostate cancer inevitably comes with a sense of shock and even fear. It can be an overwhelming and confusing time with the overriding question often being “What now?”. First off, take a deep breath or two to assist with keeping the panic at bay. Remember that most prostate cancers are slow growing, meaning that you likely don’t have to make all of your decisions immediately. Take time to consider the following suggestions:
Educate yourself
If possible read up on prostate cancer or speak to other prostate cancer patients in order to improve your understanding of the disease as this can be helpful in separating fact from fiction. It is important that you deal with fact. Be aware of “Dr Google” as reading up on medical facts without the requisite medical knowledge can be alarming and confusing.
Prepare for your next doctor’s appointment
Your doctor will likely cover the specifics of the cancer that you have and will undoubtedly tell you about treatment options which could include active surveillance (‘watching and waiting’), surgery, radiation therapy, hormone therapy, chemotherapy or even a combination of these . This can be a lot of information to take in at once so, if possible, have a notepad and pen with you so that you can jot down notes that you can look over later.
If possible take a friend or family member along with you. Not only does this provide you with some support but having another listening ear can also be helpful when there is a lot of information to absorb.
Have a list of questions written down that you would like to ask your doctor. These could include:
- Is the cancer localised or has it spread to other parts of the body (metastatic prostate cancer)?
- Is the type of cancer that I have curable?
- Will further tests be needed? If so, which tests? And who will be available to explain to me what the results mean?
- What are all my treatment options?
- What factors should I consider when choosing a treatment?
- What is your experience with these treatments?
- When can the treatment begin and for how long will it last?
- What are the possible side effects of and/or risks associated with the various treatment options? Could these include incontinence, erectile dysfunction, loss of sex drive, pain? If so, how do I best manage these?
- How will the treatment affect my quality of life?
- If surgery is an option what all does the surgery involve and what would the hospital stay entail?
- Is active surveillance an option for me? If so what does it involve and how often will I need to be checked? What should I be looking out for?
- What if the cancer spreads?
- What other health professionals will be involved in my treatment and care – oncologists, nuclear medicine physicians, psychologists, physiotherapists, anesthaesiologists?
- What outcomes can I realistically expect from a specific treatment option?
Request a copy of all your lab results and any other tests that are done and keep these in a safe place. They are useful to have if you want another opinion and if you do any of your own research. However always speak to your specialist before you reach any conclusions on your own.
Find the right doctor
If you have a private medical aid you should try to find specialists that you are comfortable with and that you feel you can trust. You’re going to see him/her frequently over an extended period of time, you may as well like him and feel a ‘right fit’ with him.
Initially you will probably be referred to a urologist who will make the diagnosis. Depending on how the cancer is going to be treated you may also be referred to an oncologist, a radiation oncologist or even a nuclear medicine physician. Other healthcare professionals like physiotherapists and sexologists might also assist you at different stages of your treatment.
If you have a family doctor/GP they can help you find a specialist.
Seek a second opinion if necessary
Your health and your treatment are your responsibility. If you are not happy with the advice you are receiving from your doctor seek a second opinion. Do not be concerned about possibly offending your doctor, it is your right to seek out the help you feel you need.
Don’t try and do it alone
This can be a scary time and it is important to draw on all the resources and support structures available to you. Talk to someone – whether it be your partner, a friend, a family member or a professional such as a nurse or a counsellor or a psychologist. Share what you are thinking and feeling. You may well be feeling anxious about the future and about the impact of your illness on the relationships with the people close to you. Talking about these things is not a cure but it will definitely help you feel less burdened and will assist you in processing the confusing thoughts and feelings.
You may well find that your loved ones are as confused and anxious as you are. Their personal discomfort and fear might mean that they find it too difficult to even acknowledge your illness, let alone talk about it. They will not necessarily know how to support you. Be direct and honest about what you need from them and how they can help you. Don’t expect them to be able to read your mind.
Join a support group or talk to a prostate cancer survivor
Becoming part of a group of men who are going through a similar experience to you can be tremendously helpful. It provides you with an opportunity to ask questions and express concerns to people who understand exactly what you are going through. The Prostate Cancer Foundation of South Africa runs an email support group.
Take care of yourself
Do whatever you can to maintain your health. Explore stress management and relaxation techniques. Eat well, remain as active as possible, and get sufficient sleep. Set your own pace. Yes, you have cancer but try not to allow the diagnosis to define you. Pursue your hobbies and interests and maintain your friendships. Talk about things other than your disease. Set yourself achievable goals, schedule things that you can look forward to.
Seek emotional help if you need it
If you continue to feel overwhelmed and are simply not able to shake anxious and depressive thoughts and feelings, seek help from a professional. Getting help is a sign of strength. It is important to take control of the things that you can take control of.
Treatment options for localised prostate cancer
Updated 28 June 2024
If you have been diagnosed with localised prostate cancer there may be various treatment options available to you. Prostate cancer that is diagnosed when it is still localised can be cured. Before deciding on what treatment will be best suited to you, your doctor should assess your life expectancy, health status, frailty and co-morbidities. If your life expectancy is less than 10 years you will be unlikely to benefit from active treatments.
The decision on what treatment will be best for you should be made jointly by you and your doctor. You should be fully informed of all treatment options available to you for your stage of prostate cancer, even if these are not provided by the specialist that you are consulting. You need to ensure that you fully understand the advantages and disadvantages of all the treatment options and their potential impact on your quality of life, in order to make an informed decision. Prostate cancer is usually a slow growing type of cancer, so you should take your time to understand the side effects of the different treatment options before you make your decision. It’s a good idea to speak to other men who have been in your position before you make your decision. You can do this by joining the Prostate Cancer Foundation’s email support group which is made up of men who have had various treatments.
Treatments options include monitoring the cancer or active treatments
Monitoring the cancer
- Active surveillance
- watchful waiting
Surgical treatments
- Open radical prostatectomy
- Laparoscopic prostatectomy
- Robotic assisted Laparoscopic prostatectomy
Radiation Treatments
- Radiotherapy options include
- External beam radiotherapy (EBRT)
- Brachytherapy (BT)
- A combination of EBRT, BT and androgen deprivation treatment
References:
1 Mutambirwa S, Coetzee L, Adam A et al. Prostate Cancer Foundation screening guidelines. Available at: https://prostate-ca.co.za/for-healthcare-professionals/.
ACTIVE SURVEILLANCE FOR LOCALISED PROSTATE CANCER
Updated 28 June 2024
Active surveillance aims to avoid unnecessary treatment and spare men from the side effects of these. Men are closely monitored with the objective of intervening timeously if there is disease progression to ensure that active treatments are still potentially curative.
Patient selection for active surveillance
Not all types of localised prostate cancer are suitable for active surveillance. Only men with low risk disease or favourable intermediate risk disease with no adverse risk features are suitable candidates.
Factors that may exclude men as candidates for AS include:
- extensive disease on MRI
- high PSA density
The following features found on the biopsy also mean that these men are not suitable candidates:
- predominant ductal carcinoma (including pure intraductal carcinoma)
- cibriform histology
- sarcomatoid carcinoma
- small cell carcinoma
- extra capsular extension
- lymph node vesicle invasion in needle biopsy
- Perinural invasion
- High risk disease
For men with very low risk disease, the 2024 NCCN guidelines now recommend that active surveillance should be the treatment of choice. The NCCN define very low risk disease as; PSA level <10 ng/mL, 3 prostate biopsy fragments/cores positive, <51% cancer in each fragment/core, and a PSA density of 0.15 ng/mL/g.) If you do choose active surveillance, you will need to be regularly monitored to ensure that any disease progression is picked up so that an active treatment can be given before the cancer spreads. The NICE protocol is one way of monitoring patients on active surveillance
| Timing | Test |
| When starting active surveillance | Multiparametric MRI if not previously performeda |
| Throughout active surveillance | Monitor changes to the PSAb |
| Year 1 of active surveillance | Every 3–4 months: measure PSA
Every 6–12 months: perform a digital rectal examination (DRE)c At 12 months: do a prostate biopsy |
| Years 2–4 of active surveillance | Every 3–6 months: measure PSA
Every 6–12 months: perform DRE |
| Year 5 and every year thereafter until active surveillance ends | Every 6 months: measure PSA
Every 12 months: perform DRE |
aIf there is concern about clinical or PSA changes at any time during active surveillance, reassess with multiparametric MRI and/or rebiopsy.
bMay include PSA doubling time and velocity.
cShould be performed by a healthcare professional with expertise and confidence in performing DRE.
Advantages of active surveillance
- You avoid the side effects of active treatments which can significantly affect your quality of life
- Active surveillance won’t affect your everyday life as much as active treatment might
- If tests show that your cancer might be growing, you can still have active treatments that aim to cure your cancer
- In a clinical trial called the ProtecT trial, the number of men with very low risk prostate cancer who died after 10 years following active surveillance compared to men who had a prostatectomy or radiation therapy was very similar
Disadvantages of active surveillance
- You will need to have more prostate biopsies
- Your general health could change, which might make some treatments unsuitable for you if you did need them
- Some men struggle with the anxiety of knowing that they have untreated cancer in their body
- In a small percentage of men who choose active surveillance the cancer spreads spreads , which means that it may no longer be curable
- In a trial comparing men who had low risk prostate cancer after 15 years, more men in the active surveillance group developed distant or regional node metastases compared to men who had a radical prostatectomy or radiation therapy:
9.4% compared with 4.7% in the radical prostatectomy group and 5.0% in the radiation therapy group
References:
1 Mutambirwa S, Coetzee L, Adam A et al. Prostate Cancer Foundation screening guidelines. Available at: https://prostate-ca.co.za/for-healthcare-professionals/.
2 Schaeffer EM, Srinivas S, Adra N, et al. Natl Compr Canc Netw 2024;22(3):140–150. Prostate Cancer, Version 3.2024 Featured Updates to the NCCN Guidelines.
Surgical Treatment for Localised Prostate cancer
Compiled July 2020
Surgery to remove the prostate is called a radical prostatectomy. The entire prostate gland, the seminal vesicles and some adjacent tissue are removed during surgery. In patients with intermediate or high risk localised prostate cancer, some of the lymph nodes may also be removed.
One of the advantages of surgery is that the entire prostate, the seminal vesicles and some of the surrounding tissues are sent to a pathology laboratory and analysed. This provides an opportunity for the prostate cancer to be restaged (pathologic staging). This type of staging is more accurate than clinical staging and you may be given a new Gleason score and tumour stage. If the pathologic staging and the surgeon’s observations show that the cancer is more aggressive than the original biopsy results showed, then your cancer may be reclassified as locally advanced and your urologist may recommend additional treatments.
Prostate cancer surgery is a major operation and, as with all surgery, there are risks that men need to be aware of. These include complications from a general anaesthetic, blood loss and the need for a blood transfusion (this is more common with open surgery), pulmonary embolism and wound infection.
The challenge with prostate cancer surgery is to remove all of the cancer whilst minimising damage to the nerves that enable men to have erections and also preserving the structures and nerve supply that are involved in bladder control (continence). Part of the procedure involves cutting the urethra just below the bladder in order to remove the prostate gland. This results in the removal of one of the sphincters (the internal urethral sphincter) that assists with bladder control (continence). The urethra is reattached to the bladder after the prostate has been removed and a catheter is kept inserted to allow the join to heal without forming scar tissue (which can result in narrowing of the tube). The catheter is a tube that drains urine from the bladder through the penis and into a bag. The catheter may be kept in place for a few days or weeks depending on the type of surgery. The two tubes carrying sperm from the testes (vas deferens) are also cut so men will be infertile after the procedure.
Nerve-sparing surgery
There are two main nerve bundles running along the sides of the prostate. These are the nerves that enable a man to have erections and they also play a role in bladder control (urinary continence). Urologists will try to preserve the nerves (a nerve-sparing prostatectomy) but this is not always possible. If the cancer has invaded the nerves they have to be removed. Even if the nerves are not removed there is a chance that they may be damaged during the surgery.
This is why erectile dysfunction is a common side effect of surgery. Full recovery of erectile function is more likely in younger men who had good erectile function before surgery and where the nerves on both sides of the prostate have been preserved. Recovery of continence is also significantly better in men who have had a nerve sparing procedure.
Types of radical prostatectomies available
Irrespective of the type of surgery you undergo, research has consistently shown that the best outcomes are achieved by surgeons who are doing high numbers of prostatectomies.
Open radical prostatectomy (ORP)
This is the traditional way that a radical prostatectomy is done. It is still the most common type of surgery performed in the public sector. Access to the prostate is either through the abdomen (retropubic approach) or the perineum (the area between the scrotum and anus). This type of a prostatectomy is the most invasive as the surgeon opens up the body and operates directly. It can result in blood loss that may require a blood transfusion. This surgery results in a longer hospital stay and recovery period than that with laparoscopic surgery and a robotic-assisted prostatectomy.
Laparoscopic radical prostatectomy (LRP)
With this type of surgery the surgeon makes small incisions across the stomach through which the surgical tools and a camera are inserted. This is why it is commonly known as “keyhole” surgery. The surgeon views the procedure on a video monitor and uses special long-shafted instruments to perform the surgery.
This is far less invasive than open surgery resulting in less blood loss, fewer blood transfusions, a shorter hospital stay and a quicker recovery. The hand movements of the surgeon is restricted because of the way that laparoscopic instruments are fixed at skin level. This type of surgery requires a long learning period for surgeons and the precision, articulation and vision required to perform it means that it is limited to a few surgeons.
Robotic-assisted radical prostatectomy (RARP)
To read more about what expect after you have had a robotic prostatectomy click on the link below:
https://www.woscan.scot.nhs.uk/wp-content/uploads/291393-Robotic-Discharge.pdf
As with normal laparoscopic surgery described above, small incisions are made in the stomach through which cameras and instruments are inserted. However, there are a number of differences with robotic surgery compared with traditional laparoscopic surgery. RARP expands the surgeon’s capabilities as outlined below:
The surgeon’s operating position
With traditional laparoscopic surgery and open surgery, the surgeon physically stands over the patient and operates through the incisions using long-shafted instruments.
With robotic surgery the surgeon sits comfortably at a console away from the patient. The instruments are situated above the patient and are inserted through the incisions. This results in less fatigue for the surgeon.
Manoeuvrability of the surgical instruments
With traditional laparoscopic surgery the instruments used are long shafted instruments which provide less flexibility, dexterity and range of motion than with robotic surgery. With robotic surgery the surgeon controls the robotic instruments using natural hand and wrist movements. The instruments can rotate through 540 ° and are more mobile than the human hand. The system even filters out unpredictable movements and tremors.
Visualisation
With robotic surgery the surgeon is provided with a magnified high-definition three-dimensional view of the tissue planes, target anatomy and the neurovascular bundles.
For these reasons robotic prostatectomies have become the standard procedure in many developed countries.
Removal of lymph nodes – pelvic lymph node dissection (PLND)
If you have intermediate or high-risk localised prostate cancer then your urologist might remove some of the lymph nodes. In some cases they may only remove lymph nodes in the close proximity to the prostate. Where there is a higher risk of the cancer having spread they may remove lymph nodes further afield, this is called an extended pelvic lymph node dissection. The removed lymph nodes are sent to a laboratory to be checked for prostate cancer. Knowing if the cancer has spread to the lymph nodes is important as this can assist with planning additional treatments. If the laboratory results show that the cancer has spread extensively to the lymph nodes, you may require additional treatment after the surgery in the form of androgen deprivation therapy.
Side Effects of pelvic lymph node dissection
The lymph nodes drain tissue fluid, so removing them can result in a build up of tissue fluids (oedema) in areas where drainage no longer takes place. This is more likely if an extended pelvic lymph node dissection has been performed. Patients may suffer from leg oedema and in some cases oedema of the scrotum and penis.
Monitoring treatment outcomes
Your cancer will be restaged after the surgery based on the laboratory results (see article on prostate cancer staging). This will provide a better indication of how aggressive the cancer is. The laboratory will also report on the surgical margins ie. the presence of (positive surgical margin) or absence (negative surgical margin) of cancer cells in the edge of the tissue surrounding the removed tumour. A negative margin is an indicator that all the cancer was removed. A report of positive surgical margins is not a 100% accurate predictor that the cancer has spread, as several factors can cause “spillage” of cancer cells into the adjacent tissue that is examined buy the laboratory.
After having a radical prostatectomy the PSA levels should drop to undetectable levels (< 0.01 ng/mL) within 6 weeks as there should no longer be any prostate cells still in the body to produce PSA. This is called the PSA nadir. Failure to reach a PSA level of 0.01 or a rising PSA could mean that there are still some prostate cancer cells in the prostatic bed (the area where the prostate was) and/or there are microscopic deposits of prostate cancer cells (micro metastases) in the body. This is called biochemical recurrence. In this case your urologist may recommend additional treatment with external beam radiation therapy to target prostate cancer cells remaining in the prostatic bed or hormone therapy to stop any other cancer cells in the body from growing.Side effects from a radical prostatectomy
Side Effects
Urinary Incontinence
Many men will experience problems with bladder control (continence) after a prostatectomy. The leaking of urine is called urinary incontinence. It is one of the most irritating and embarrassing side effects that men have to deal with. Most men eventually regain control of their bladder but it can it can take up to a year.
There are two types of incontinence that men can experience after a prostatectomy:
- Stress incontinence is leaking of urine after exertion. Activities or exertion that cause leaking can be as mild as coughing , sneezing or just shifting position. This is the most common type of incontinence after a prostatectomy.
- Urge incontinence occurs when you feel a sudden urge to urinate but you can’t “hold it in” until you get to a toilet.
Click on the link below to read one man’s experience with incontinence:
https://www.pcf.org/c/long-wet-road-back-normal/
Why does urinary incontinence occur after a prostatectomy?
With all the different types of surgery, one of the sphincters (the internal urethral sphincter situated in the bladder neck) is removed. The prostate also plays a role in continence and is also removed. Bladder control is then dependant on one sphincter (the external sphincter) which is situated just below the prostate. This is the strongest and most important of the three continence mechanisms. With two of the mechanisms that normally help with continence having been removed, continence is now reliant on one sphincter.
There are several factors which can affect how quickly and how well you recover bladder control (continence):
Damage to the external sphincter
The external sphincter sits just below the prostate and is the muscle that you use to control your flow of urine. The supporting structures such as nerves, blood supply and the muscle surrounding the sphincter can be damaged during surgery and can take up to a year to fully recover. Men who have problems with urinary continence before the procedure are also more likely to experience problems after the surgery.
Nerve-sparing vs non-nerve-sparing prostatectomy
There are 2 nerve bundles around the prostate that play a role in controlling the flow of urine and erectile function. Urologists will try to do a nerve-sparing procedure in order to try and keep these intact but this is not always possible. Men who have a nerve-sparing prostatectomy are likely to regain bladder control in half the time of men who had a non-nerve-sparing prostatectomy. (5.3 months compared to 10.9 months).
The type of surgery
There is evidence to show that continence rates are better after a robotic prostatectomy than with other types of surgery. Surgeons are better able to see the nerves due to the magnification provided by the robotic cameras and they have more manoeuvrability due to the degree of movement provided by the robotic instrumentation. This allows for greater precision and preservation of the nerves that supply the external sphincter. In terms of recovery time, some studies have shown that men are continent 44 days after robotic surgery compared to 160 days after traditional open surgery.
The length of the urethra after surgery
The urethra is cut and reattached to the bladder. If the remaining length of the urethra is less than 12mm after surgery this can affect continence.
Age
As men get older the muscles around the sphincter get weaker which means that they are at increased risk for incontinence after surgery.
Obesity
Patients with a body mass index (BMI) over 30kg/m2 are three times more likely to have problems with incontinence after surgery.
Sexual side effects
(See section on managing sexual side effects after active treatments)
Ejaculation problems
Men who have undergone a radical prostatectomy will no longer be able to ejaculate. This is because the prostate and seminal vesicles make up most of the ejaculate (seminal fluid) and they are removed. The tube that carries semen from the testes is also tied off, although semen only makes up about 2% of the ejaculate. Men who want to still father children should consider having their semen frozen and stored in a sperm bank before the procedure.
Orgasmic function
Although men will be unable to ejaculate after a prostatectomy they will still be able to experience the sensation of orgasm. The quality of orgasm, however, may be affected. Some men will experience painful orgasms although this tends to improve over time. Men who have a robotic prostatectomy are less likely to experience this problem.
Erectile dysfunction
This is a common side effect that can occur after all active treatments for prostate cancer. The nerves and blood vessels responsible for erections can be damaged by the surgery and can take months to heal. Men who have erection problems before a prostatectomy are more likely to have problems after the surgery. Men who have had a nerve-sparing prostatectomy are more likely to recover erectile function. For men who want to recover erectile function, it is essential that that they begin penile rehabilitation as soon as possible after surgery (see section on managing sexual side effects after active treatments).
Climacturia
This is the loss of bladder control (continence) whilst having an orgasm and it occurs in about 30% of men who have had a prostatectomy. The problem normally improves over time and patients who have had a robotic prostatectomy recover more quickly from this condition. Emptying your bladder before you have sex and using condoms can help. Physiotherapists who work with pelvic dysfunctions can also assist with pelvic floor exercises.
Long term complications
Urinary incontinence and erectile dysfunction are the most common long term complications after a radical prostatectomy. Some men experience penile shortening although this usually corrects as healing progresses and scar tissue softens.
Advantages of Surgery
- If the cancer is contained in the prostate, men will have the reassurance that it has been removed from the body
- Because the prostate and seminal vesicles are removed from the body and sent for laboratory analysis, surgery provides the best way to assess how aggressive the cancer is and the cancer can be more accurately restaged (pathologic staging)
- Men who have an enlarged prostate (benign prostatic hyperplasia) will no longer have symptoms for this condition as the prostate is removed
- Assessing treatment success is quick, as PSA levels should drop to undetectable levels soon after treatment, whereas this can take up to 2 years with radiotherapy
- It is easy to monitor patients to check if the cancer has returned by using PSA tests
- If the treatment has failed, radiotherapy can be used as a backup treatment (salvage therapy)
Disadvantages of Surgery
- A prostatectomy is a major operation and there is a risk of blood loss and the need for a blood transfusion. However, this is less likely to occur with laparoscopic and robotic surgery which also have the benefit of a shorter hospital stay and quicker recovery time
- Patients will be discharged with a urinary catheter which will have to be removed 1 to 2 weeks after being discharged
- Many patients experience urinary incontinence after the catheter is removed. This can take weeks or months to completely clear up, although many patients have acceptable control within the first 3 months
References
(1) Cao L et al. Robot-assisted and laparoscopic vs open radical prostatectomy in clinically localized prostate cancer: perioperative, functional, and oncological outcomes. A Systematic review and meta-analysis. Medicine (2019) 98:22.
(2) Kirby RS, Patel M. Fast Facts: Prostate Cancer. Eight Edition 2014. Health Press Limited
(3) Leow, Jeffrey J. et al. Systematic Review of the Volume–Outcome Relationship for Radical Prostatectomy. European Urology Focus, Volume 4, Issue 6, 775 – 789.
(4) Hoyland K et al. Post–Radical Prostatectomy Incontinence: Etiology and Prevention. Reviews in Urology. 2014;16(4):181-188
(5) Jaffe WI et al. Urinary Incontinence After Prostate Cancer Surgery & Radiation. Available at:
www.oncolink.org/cancers/prostate/support-and-survivorship/side-effects/urinary-incontinence-after-prostate-cancer-surgery-radiation-therapy
(6) Mottrie et al. Balancing continence function and oncological outcomes during robot-assisted radical prostatectomy (RARP)
(7) Singla N et al. Post-prostatectomy incontinence: Etiology, evaluation, and management. Turkish Journal of Urology; 40(1): 1-8
(8) For Healthcare professionals: Prostate cancer essentials: Localised prostate cancer. Prostate Cancer UK.
(9) McLeod DG. The Effective Management of Biochemical Recurrence in Patients With Prostate Cancer. Reviews in Urology. vol. 7 suppl. 5 2005
(10) Skove SL et al. Timing of PSA nadir after radical prostatectomy and risk of biochemical recurrence. Urology. 2017 October ; 108: 129–134
Radiotherapy for Treating Localised and Locally Advanced Prostate Cancer
Radiotherapy
Radiotherapy or radiation therapy refers to the use of high energy X- rays used to treat cancer. These high energy X- rays are different from diagnostic X rays such as a CT scan where the X- rays are of a lower energy. Radiation therapy works by destroying a cancer cell’s DNA which prevents the cells from reproducing and causes cell death. The aim is always to deliver a high enough dose to the cancer tumour to maximise disease control, whilst keeping the dose that reaches normal healthy tissues as low as possible to minimise side effects and complications.
Radiotherapy treatments are managed by medical specialists called radiation or clinical oncologists. They are assisted by medical physicists who help with the planning of the treatment and by radiation therapists who set-up the patient for the treatment and operate the machinery required to administer the treatment.
The two types of radiotherapy available in South Africa to treat localised and locally advanced prostate cancer are external beam radiation and brachytherapy.
Cyberknife which uses stereostatic body radiation therapy (SBRT) and computer-assisted image guidance to deliver very high doses of radiation to the tumour, is not yet available in South Africa.
External beam radiation therapy (EBRT)
This treatment option is completely non-invasive. There is no surgery involved, so it is a suitable option for men who do not want any surgery or who are not suitable for surgery because of other health issues.
The treatment is done at a special facility using a machine called a linear accelerator. The machine delivers high energy X-rays to the targeted area.
The challenge with radiotherapy is to deliver a high enough dose to the prostate whilst avoiding damage to the bladder and the rectum. The beam is moved in an arc around the prostate so it will pass through structures like the bowels at some point during the treatment session.
For localised prostate cancer
For low risk localised prostate cancer the whole of the prostate gland is treated but not the seminal vesicles.
For locally advanced prostate cancer
For T3 disease where the cancer has spread outside of the prostate, the seminal vesicles will also be treated. In some patients, the seminal vesicles are close to the rectum which means that it will fall in the treatment area. This will increase the likelihood of gastro-intestinal side effects (bowel side effects).
For intermediate or high risk prostate cancer
Hormone therapy will be given before and/or together with the EBRT. This helps to reduce the tumour size and make the cancer cells more sensitive to the radiation.
Treating the pelvic lymph nodes
Some oncologists may also treat the pelvic lymph nodes if they suspect that the cancer has spread to them. This means that the treatment area will be bigger and that there will be an increased likelihood of gastro-intestinal side effects (bowel side effects).
Types of external beam radiation therapies
With both types, a planning session will be done before the treatment sessions starts. Scans are taken to map the size, shape and location of the prostate so that the exact treatment area will be targeted by the radiation beam. This will help to avoid damaging healthy tissue.
At some centres, where thelinear accelerator does not have a CT scanner attached, patients may have to have a few radio-opaque seeds implanted into the prostate so that a normal X-Ray machine can be used for set-up to ensure that the beam is targeted at the prostate.
Three small tattoos will be marked out on your abdomen. These are used to get you in the correct position for each treatment.
3D conformal radiotherapy (3D-CRT)
This system allows the beam to be adjusted to the shape and size of the prostate in all three dimensions. However, the strength of the beam cannot be controlled so all areas of the prostate are treated with the same dose.
Intensity-modulated radiotherapy (IMRT)
This is a newer system than (3D-CRT). The advantage is that the strength of the beam can be adjusted. For example, a lower intensity can be used when the beam passes through the rectum which helps to reduce side effects. Treatment sessions can take longer depending on the machine.
How long does the treatment take?
With the traditional method, small doses of radiation (1.8-2Gy) are delivered daily, Monday to Friday over a period of 7 to 8 weeks until the prescribed dose of 74GY is reached. Each treatment takes about 15 minutes.
Hypo-fractionation treatment
This is a newer EBRT technique that involves delivering a higher daily dose (3Gy) over 4 to 5 weeks until the prescribed dose of 60Gy has been reached. The convenience of a shorter period is making this a popular treatment option.
Treatment set-up
One of the challenges with EBRT is that the beam has to be aimed as accurately as possible at the prostate to insure that the radiation is directed at the targeted area. The problem is that the prostate can move from day-to-day due to pressure from the bladder or the rectum, depending on filling and emptying, so patients may be instructed to try and keep this as consistent as possible.
Patients will also be immobilised for the duration of the treatment and adjustments will be made daily using the machines built-in CT scanner or other imaging methods. This is called Image Guided-Intensity Modulated Radiotherapy (IG-IMRT).
Precision is a key factor with external beam radiation and is even more critical when using higher -dose treatments.
Monitoring treatment outcomes
After the treatment is complete you will be monitored by your oncologist to check if the cancer returns or not. The PSA blood test will be used but it can take up to 2 years to drop to its lowest level. Some patients who have EBRT get a sudden temporary rise in their PSA levels and then it drops down again. This is called PSA bounce and it doesn’t mean that the cancer is growing again.
Once the PSA has reached its lowest level, (nadir) an increase of 2ng/ml is regarded as disease recurrence. eg going from 0.75 to 2.75. This is referred to as biochemical recurrence and it is a sign that the cancer is growing.
Another definition of biochemical recurrence is if there are 3 consecutive rises in the PSA when it is measured at least 3 months apart.
Side Effects of External Beam Radiation
Oncologists have to try and achieve a balance between providing a strong enough dose to destroy the cancer cells whilst minimising the radiation to the surrounding organs. Side effects occur when healthy tissue is damaged by the radiation. Oncologists refer to this as toxicity. The healthy tissue may heal but this can take time.
Short term side effects may begin 2-4 weeks after starting treatment and can last up to 4-8 weeks after treatment. The radiation can cause irritation and inflammation of the bladder (cystitis) and the rectum (proctitis). This can cause urinary and gastro-intestinal side effects. Some patients experience late side effects that only occur after the treatment is completed.
Urinary side effects include:
- the need to urinate frequently
- having to get up at night to urinate
- a sudden urgent need to urinate
- difficulty urinating or slow urination (obstruction)
Gastro-intestinal side effects (bowel side effects) include:
- loose stools (diarrhoea)
- bloody stools
- bleeding from the anus
- needing to defecate frequently
- cramps
- an urgent need to defecate
Sexual side effects
(See section on sexual side effects after active treatments)
All active treatments are likely to affect your sex life. Some studies show that the sexual side effects from EBRT get worse over time.
Ejaculation problems
The majority of men who have external beam radiation therapy will eventually not be able to ejaculate after treatment (anejaculation) and this gets worse over time. In one study 16% of men experienced the problem after 1 year, 69% after 3 years and 89% after 5 years.
Erectile dysfunction
This is a side effect that can occur after all active treatments for prostate cancer. Erectile function before treatment is an important factor. The dose of radiation that is delivered to structures that play a role in erections such as the penile bulb and the blood vessels appears to have an important effect on erectile function after treatment. Some oncologists have developed techniques to preserve these structures.
Long term complications
The most common long term complication of EBRT is bowel function. In one study, 5 years after treatment 33% of men reported that they are still bothered by an urgent need to defecate. 24% of the men also reported being bothered by slow or difficult urination. Some men will have erectile dysfunction but this can also be related to ageing and other comorbid conditions.
Advantages of External beam radiation therapy (EBRT)
- The treatment is completely non-invasive so it can be given to men who are not fit for surgery or don’t want surgery
- There are none of the problems or complications that can occur with major surgery
- Most men can continue working whilst having the treatment so there is no need to take time off work (although some men will experience fatigue)
- There is no hospitalisation
- The treatment itself is pain free
Disadvantages of External beam radiation therapy (EBRT)
- This is a time consuming treatment that involves daily visits during the week to a specialised facility for 4 to 8 weeks depending on the treatment regime
- The prostate is not removed as with surgery so restaging the cancer is not possible as it is with surgery
- Using the PSA levels to determine if the treatment has been successful can be difficult, as it can take up to 2 years to drop to its lowest level. Some men get aPSA bounce (temporary rise in PSA levels) which further confuses the issue. If men have hormone therapy together with the EBRT, this will also affect the PSA score.
- If the cancer recurs, further radiation is generally not possible
- If the cancer recurs, salvage surgery is possible, but it is far more difficult than in men who have had no radiation treatment and it has a higher rate of complications
- The gastrointestinal side effects (bowel problems) are higher than with other active treatments
- As with other active treatments, there are urinary and sexual side effects that can have a significant impact on a man’s quality of life
- The beam has to travel through healthy tissue which exposes it to some radiation leading to possible side effects
References
1 Kirby RS, Patel M. Fast Facts: Prostate Cancer. Eight Edition 2014. Health Press Limited
2 External beam radiation. Prostate Cancer UK. Availble at: https://prostatecanceruk.org/prostate-information/treatments/external-beam-radiotherapy
3 Dang et al. Image-guided radiotherapy for prostate cancer. Transl Androl Urol 2018;7(3):308-320
4 Prostate cancer essentials: Localised prostate cancer. Prostate Cancer UK
5 Potosky AL et al. Five-Year Outcomes After Prostatectomy or Radiotherapy for Prostate Cancer: The Prostate Cancer Outcomes Study. Journal of the National Cancer Institute, Vol. 96, No. 18, September 15, 2004
6 Samlali H et al. Prospective evaluation of a specific technique of sexual function preservation in external beam radiotherapy for prostate cancer. Br J Radiol 2017; 90: 20160877.
Low Dose Seed Brachytherapy
(High dose rate temporary brachytherapy is not commonly available in South Africa and is therefore not discussed as a treatment option).
Low dose seed brachytherapy involves the permanent insertion of tiny radioactive seeds which are about the size of a rice grain into the prostate gland. These emit low doses of radiation within the prostate over about 3 months, although the seeds remainbiologically active for about 9 months.
The advantage of low dose radioactive seeds is that the radiation decreases in strength as it moves away from the source. This means that the structures surrounding the prostate such as the bladder and rectum are less affected by the radiation.
Assessing patients suitable for brachytherapy
A urologist will have performed the biopsy. This will have enabled the urologist to determine the size and position of the prostate and the stage of the prostate cancer.
If the patient has a very large prostate, then some urologists may use androgen deprivation therapy for 2 to 5 months to shrink the prostate.
Patients who have had a transurethral resection of the prostate (TURP) as a treatment for an enlarged prostate will have to be carefully assessed as performing brachytherapy on these patients is more complicated and technically difficult. If the TURP procedure has damaged the urethra then brachytherapy might not be possible.
Some patients have pelvic anatomy that can make the procedure more difficult.
Patients who have had previous radiation treatments to the pelvic area will have to be carefully assessed as this can result in increased side effects brought about by the additional radiation introduced by brachytherapy.
A simple self-report questionnaire called the International Prostate Symptom Score (IPSS) should be given to all patients to determine if there are urinary symptoms that could be made worse by undergoing treatment with brachytherapy. Men who have existing urinary problems or who score greater than 12 on the IPSS are at increased risk of urinary incontinence and other urinary problems if they have brachytherapy.
For low risk localised prostate cancer
(From American Brachytherapy Society consensus guidelines)
If your Gleason score ≤ 6
PSA<10 ng/mL Tumour stage T1 or T2a Brachytherapy can be used as a single treatment
For intermediate risk localised prostate cancer
(From American Brachytherapy Society consensus guidelines)
If your Gleason score ≤ 7
PSA<20 ng/mL Tumour stage T2b or T2c Brachytherapy can be used as a single treatment but some specialists may combine the treatment with external beam radiation therapy and/or androgen deprivation therapy
For High Risk localised prostate cancer
(From American Brachytherapy Society consensus guidelines)
If your Gleason score is 8 to 10
PSA > 20 ng/mL
Tumour stage T3a
Brachytherapy cannot be used as a single treatment
The treatment will need to be combined with external beam radiation therapy
The inclusion of androgen deprivation therapy is optional but there is limited data on whether it improves the treatment outcomes
The Procedure
A multidisciplinary team of healthcare professionals are involved in planning and administering the treatment. A radiation or clinical oncologist will decide on the number of brachytherapy seeds required and will plan the treatment together with a medical physicist.
Brachytherapy is done in theatre under general anaesthetic either as a day procedure or an overnight admission. The radiation/clinical oncologist and medical physicist will both be in the theatre for the procedure. They will ensure that the seeds are placed in the correct position according to the treatment plan and that surrounding organs are protected from high doses of radiation in order to limit side effects. The urologist may be involved with the insertion of the needles and, in some cases, placement of the seeds.
For the procedure a trans-rectal ultrasound probe is inserted up the rectum which provides an image of the prostate. A Foleys catheter is inserted through the penis to the bladder so that it can be clearly seen. A reference grid is placed above the ultrasound probe and the needles are inserted through the perineum (the area between the anus and scrotum) to the different parts of the prostate as per the treatment plan via the grid. The seeds are deposited through the needles into the prostate. The number of seeds used will depend on the size of the prostate.
After Treatment
Radioactivity
The brachy seeds that are implanted in your prostate release low doses of radiation and a very low amount of the radiation may be present outside of your body. Although this amount of radiation is small and not considered dangerous, as a precaution after the treatment, men are advised to not spend extended periods of time close to pregnant women or young children for the first two months. Very rarely men may pass a seed when urinating.
Returning to work
There is no prescribed rest period, so theoretically you can return to work the day after the procedure.
Exercising
There is no time restriction on when you can start exercising except for cycling. The perineum will need time to recover so no cycling for at least 6 to 8 weeks.
Sex
There is no time restriction on sexual activity so you can have sex as soon as you want to. There is a very small chance of a radioactive seed being ejaculated so for the first few times that you have sex you should wear a condom. Some men report pain with erections and ejaculation after the procedure. If you want to remain sexually active you should stimulate yourself a few times a day to get erections as this helps to restore circulation and nerve function.
Monitoring treatment outcomes
It can take up to 5 years for the PSA to reach its lowest point after brachytherapy so it won’t be possible to determine if you are cancer-free until the PSA reaches its lowest point. This is called PSA Nadir and ideally it should be below 0.5 ng/mL. 30 % to 40% of men get a sudden temporary rise in their PSA levels and then it drops down again. This is called PSA bounce and it doesn’t mean that the cancer is growing again but it can be confusing. Failure to reach a PSA level of 0.5 ng/mL is associated with an increased risk of recurrence.
Once the PSA has reached its lowest level, an increase of 2ng/ml is regarded as disease recurrence. For example, going from 0.75 to 2.75. This is referred to as biochemical recurrence. Another definition of biochemical recurrence is if there are 3 consecutive rises in the PSA when it is measured at least 3 months apart. If this happens, it may be necessary to have a biopsy and other tests to check if the cancer has spread. After brachytherapy only a transperineal biopsy can only be done.
Side Effects of brachytherapy
Side effects occur when healthy tissue is damaged by the radiation. Oncologists refer to this as toxicity. The healthy tissue may heal but this can take time.
Short term side effects may begin 2-4 weeks after receiving treatment and can last up to 4-8 weeks after treatment. The radiation can cause irritation and inflammation of the bladder (cystitis) and the rectum (proctitis). This can cause urinary and gastro-intestinal side effects. Some patients experience late side effects that only occur after the treatment is completed.
Urinary side effects are often delayed until 1 to 4 months after treatment and are most commonly obstructive or irritative in nature. Most symptoms will resolve within one year.
Obstructive urinary symptoms
- a percentage of patients (5 to 28%) get complete urinary obstruction (unable to urinate). It is essential to get immediate medical help for this. The problem is easily treated by insertion of a catheter
- straining to urinate
- taking long to urinate
- a feeling of incomplete emptying of the bladder after urinating
- dribbling or a weak stream
Irritative urinary symptoms
About 50% of men experience symptoms as a result of irritation of the urethra. These usually resolve within one year. Irritative symptoms include:
- having to urinate frequently
- having to get up at night to urinate
- a sudden urgent need to urinate
- a burning sensation when urinating
- a weak stream
Gastro-intestinal side effects (bowel side effects) are less common from brachytherapy compared to external beam radiation and may include:
- loose stools (diarrhoea)
- bloody stools
- bleeding from the anus
- needing to frequently defecate
- cramps
- an urgent need to defecate
- pain when passing a stool
Sexual side effects
(See section on sexual side effects after active treatments)
All active treatments are likely to affect your sex life.
Ejaculation problems
There may be blood in the ejaculate in the first few weeks after the procedure. Most men who have ejaculations before treatment will continue to have them after treatment, however there is likely to be a reduced volume of ejaculate and, in some cases, no ejaculate. Some men may experience painful ejaculations. Many men will have delayed or weaker orgasms.
Erectile dysfunction
This is a side effect that can occur after all active treatments for prostate cancer. Erectile function before treatment is an important factor. With brachytherapy the dose of radiation that is delivered to structures that play a role in erections, such as the penile bulb, appears to have an important effect on erectile function after treatment so the oncologist will generally lower the dose in the seeds near to these areas.
Long term complications
Damage to the urethra from the radiation can cause it to narrow in some men. This is called a
Stricture and it makes it difficult to pass urine. This can be treated with surgery.
Men who had urinary problems before having brachytherapy or who have a large prostate are more likely to have long term urinary symptoms after brachytherapy.
Advantages of Brachytherapy
- This is usually a day procedure so you avoid hospitalisation
- Recovery from brachytherapy is quick, so you can be back at work and exercising the day after the procedure
- You do not have to have a catheter after the surgery
- There is an advantage over EBRT in that the dose is delivered at the source which minimises radiation exposure to surrounding healthy tissue.
Disadvantages of brachytherapy
- It can take 2 years for the PSA to be reliable. So you won’t know if the treatment has been successful until then
- If the treatment has not been successful, surgery can be difficult to perform and the side effects may be worse
- The prostate is not removed as with surgery so restaging the cancer is not possible as it is with surgery
- The procedure is done under general anaesthetic which always has some risk
References:
1 Davis BJ et al. American Brachytherapy Society consensus guidelines for transrectal ultrasound-guided permanent prostate brachytherapy. Brachytherapy 11 (2012) 6-19.
2 Bradley JS et al. Low dose rate prostate brachytherapy. Transl Androl Urol 2018;7(3):341-356.
3 Rukstalis et al. Treatment Options After Failure of Radiation Therapy—A Review. vol. 4 suppl. 2 2002 Reviews in Urology.
4 Steggerda MJ et al. Predicting Urinary Morbidity after Brachytherapy of Localized Prostate Cancer. European Urology Supplements 7 ( 2 0 0 8 ) 723–731.
5 Logghe P et al. Long term outcome and side effects in patients receiving low-dose I125 brachytherapy: a retrospective analysis. Outcome and side effects in brachytherapy. Vol. 42 (5): 906-917, September – October, 2016.
6 Njomnang Soh et al. Erectile function after permanent 125I prostate brachytherapy for localized prostate cancer. Basic and Clinical Andrology 2013, 23:2
7 Huyghe E et al. Ejaculatory Function After Permanent 125I Prostate Brachytherapy for Localized Prostate Cancer. Int J Radiat Oncol Biol Phys. 2009 May 1;74(1):126-32.
8 For Healthcare professionals: Prostate cancer essentials: Localised prostate cancer. Prostate Cancer UK.
9 Permanent seed brachytherapy. Prostate Cancer UL. Availble at: https://prostatecanceruk.org/prostate-information/treatments/permanent-seed-brachytherapy
- Kirby RS, Patel M. Fast Facts: Prostate Cancer. Eight Edition 2014. Health Press Limited
Metastatic (Advanced Stage) and Recurrent Prostate Cancer
When prostate cancer spreads (metastasizes) beyond the area of the prostate and starts to grow in other parts of body it is called metastatic or advanced prostate cancer. The new growths are called metastases. Doctors may also refer to the new growths as mets or secondaries. The new growths are still made up of prostate cancer cells, irrespective of where they grow in the body. At this advanced stage the cancer is unfortunately no longer curable but can be contained for a period on appropriate therapies, with the 5 year cancer specific survival for men diagnosed with metastatic prostate cancer hovering between 30 – 40%.
How Does this happen?
There are a few possible reasons as to how men end up with recurrent or metastatic prostate cancer.
1. Recurrence after initial treatment for localised or locally advanced prostate cancer
Some men who have been treated with radiotherapy or a radical prostatectomy for localised or locally advance prostate cancer experience a rise in their PSA score at some point after the treatment. This is referred to as biochemical recurrence and it is usually an indication that the cancer is growing again.
Biochemical recurrence after surgery for localised prostate cancer
In patients who have had a prostatectomy the PSA levels should fall to below 0.1 ng/ml and recurrence is defined as a rise above 0.2 ng/ml
Biochemical recurrence after radiation treatment for localised prostate cancer
In patients who have had radiation therapy a PSA rise of 2 ng/ml above nadir (The lowest PSA level reached after therapy) is considered recurrence.
The average time for metastases to develop in patients who have a rising PSA after treatment is about 8 years. In some men prostate cancer may progress without the development of metastases.
2. Men whose first diagnoses is metastatic prostate cancer
There are usually no symptoms of prostate cancer in the early stages, so if men are not being screened regularly, prostate cancer may progress to an advanced level before symptoms cause a man to seek help. Various studies have shown that men who present with prostate cancer symptoms at South African public hospitals often have advanced metastatic prostate cancer. This may be due to a lack of awareness about age appropriate screening for prostate cancer, a lack of access to screening or a lack of awareness of prostate cancer itself. This is important as early stage prostate cancer is usually only diagnosed as a result of screening and it is potentially curable.
When prostate cancer is diagnosed at the stage when it has already metastasized it called de novo metastatic prostate cancer or synchronous metastatic disease.
Understanding how prostate cancer spreads
If prostate cancer spreads outside of the prostate, the cancer cells may invade the lymph and blood vessels. These can carry cancer cells to other parts of the body resulting in the formation of prostate cancer tumours (metastases) on bone, in lymph nodes and in organs (visceral metastases).
Oligometastatic prostate cancer
This is a relatively new concept and it refers to a sub-group of patients who have relapsed after having local therapy. These patients have less metastatic sites confined to bone or lymph nodes and are therefore not considered to have full blown metastatic disease. It is thought that by using treatments that target the metastases, it may be possible to avoid or delay hormone therapy (androgen deprivation) which is required to treat patients who have metastatic prostate cancer.
How metastatic prostate cancer is staged
The staging of cancer is a way of recording how far the cancer has progressed and what structures in the body it has spread to. The TNM staging system is used:
T describes the primary tumour and how far it has spread
N describes whether or not the cancer has spread to regional lymph nodes
M describes evidence of metastatic prostate cancer
When prostate cancer spreads to lymph nodes
The lymphatic system consists of lymph vessels, lymph nodes and two collecting ducts and is part of the body’s immune system. The lymph vessels carry lymph fluid, which contains nutrients and other substances, which are returned via drainage into the blood stream to circulate back to the rest of the body. Lymph vessels also remove and transport damaged cells, cancer cells, bacteria and viruses that drain from tissues. These are then filtered out when the lymph fluid travels through the lymph nodes.
Prostate cancer tends to spread to regional lymph nodes in the pelvic area near to the prostate first. For staging purposes this is recorded as N1 and it is not classified as metastatic disease. In patients undergoing a prostatectomy the regional lymph nodes may be removed to check if prostate cancer has spread to them (pelvic lymph node dissection). If regional lymph nodes are detected using imaging tests then they may be treated with a combination of radiation and androgen deprivation therapy
If prostate cancer spreads to lymph nodes outside the pelvic area (distant lymph nodes) then this is classified as one of the sites for distant metastases and for staging purposes this is recorded as M1a. The involvement of regional lymph nodes means that a diagnoses of metastatic prostate cancer will be made and treatment for metastatic disease will be initiated.
When prostate cancer spreads to bone (bone metastases)
Prostate cancer cells have a strong affinity to spread to bone which is the most common metastatic site. Prostate cancer cells tend to spread first to the lower spine and pelvic bones and pain in this region is often a symptom of metastatic prostate cancer.
The cancer cells interact with the different types of bone cells. Most commonly the interaction is with the bone’s “builder cells” (osteoblasts) resulting in an abnormal build-up of bone. Less commonly the interaction is with the bone’s “demolisher cells” (osteoclasts) resulting in soft sections of damaged bone. Sometimes a mi
Both types of interaction cause bone weakness and increase the risk of fractures.
The presence of bone metastases is recorded as M1b for staging purposes.
When prostate cancer spreads to organs (visceral metastases)
When prostate cancer spreads to soft tissue organs other than the lymph nodes these growths are called visceral metastases. For staging purposes visceral metastases are indicated as M1c.
Men with visceral metastases generally have a worse outcome than men who only have bone metastases. Typical visceral metastatic sites are the lungs and liver which are generally affected in the late stages of prostate cancer. Most men (76%) that develop lung and liver metastases already have bone metastases.
Less common visceral metastatic sites include the brain/meninges, the thyroid gland, adrenal glands, peritoneum, gastrointestinal tract (stomach and intestine), urinary tract, ureters, urethra and kidneys, spleen or pancreas. Men with liver metastases tend to have the worst survival outcome compared to men with bone metastases or other sites of visceral metastases.
Castrate resistant metastatic prostate cancer
Unfortunately, most advanced prostate cancers treated with hormone /androgen-deprivation therapy begin to progress again within 12 to 33 months. It is thought that cancer cells that are not dependant on testosterone begin to develop, so hormone therapy that deprives the body of testosterone is no longer effective. At this point the prostate cancer is referred to as castrate- resistant prostate cancer (CRPC).
Non-metastatic (M0) castrate-resistant prostate cancer – nmCRPC
If the only sign that the cancer has become resistant to hormone therapy is a rising PSA, then the cancer is referred to as non-metastatic castrate-resistant prostate cancer and this is indicated by M0
Metastatic (M01) castrate-resistant prostate cancer -mCRPC
If imaging tests show metastases and there is a rise in PSA levels then the cancer is referred to as metastatic castrate-resistant prostate cancer and this is indicated by M1
Symptoms of metastatic prostate cancer
Pain in the pelvis and lumbar spine from bony metastases is the most common presenting symptom in men with metastatic prostate cancer.
The bone is weakened from the formation of metastases so these patients are more at risk for fractures of the spine, the hip and the neck of the femur (the long leg bone that attached to the hip joint)
In about 12% of men, tumours that form on the vertebra can cause spinal cord compression resulting in neurological symptoms such as sciatica (pain down the back of the leg) and even paraplegia.
Metastases to the lymph nodes can cause lymph node enlargement and this can result in:
- obstruction of the ureters (the tubes that carry urine from the kidney’s to the bladder
- loin pain
- swellings that can be felt
- failure of the kidney’s to produce urine (anuria)
- (swelling) of the lower limbs due to the build- up of lymph fluid ( lymphedema)
Systemic metastases can cause non-specific symptoms such as fatigue due to loss of red blood cells (anaemia) or the build-up of urea in the blood (uraemia), weight loss and muscle wasting.
Prognosis
Although metastatic prostate cancer in not curable, there are numerous treatment options that can slow the progression of the cancer and prolong life. These are discussed in the section on treatments for metastatic prostate cancer.
General health measures such as exercise and not smoking also contribute to prolongation of survival. Bone, heart and mental health also need to be addressed and should be a part of both patient and treating team’s goals.
In addition, other first degree family members may have an increased risk of developing cancers, particularly breast and prostate cancer and so should be advised about age appropriate screening for higher risk groups.
References
- Coetzee L. Metastatic Prostate Cancer. Health Press Limited 2017.
- Gandaglia G et al. Distribution of Metastatic Sites in Patients with Prostate Cancer: A Population-Based Analysis. Prostate 74:210–216, 2014.
- Barbosa FG et al. Revisiting prostate cancer recurrence with PSMA PET: Atlas of typical and atypical patterns of spread. Radiographics 2019; 39:186-212
- AJCC Cancer Staging Handbook. Seventh Edition. Springer 2010
- Douketis JD. Overview of the Lymphatic System. Merck Manual. Consumer Version. Available at: https://www.merckmanuals.com/home/SearchResults?query=lymphatic+system. (Accessed on 5th July 2016).
- Wong SK et al. Prostate Cancer and Bone Metastases: The Underlying Mechanisms. Int. J. Mol. Sci. 2019, 20(10), 2587
- Klaassen Z., The Impact of Visceral Metastasis in Prostate Cancer Patients. Available at: https://www.urotoday.com/library-resources/mcrpc-treatment/111525-the-impact-of-visceral-metastasis-in-prostate-cancer-patients.html
- Kirby RS, Patel I. Fast Facts: Prostate Cancer. Eighth edition. Health Press Limited. Jan 2014.
Treatments for Advanced Prostate Cancer
Many men will be diagnosed and treated for prostate cancer in the earlier stages. In about 30% of these men treated for localised or locally advanced prostate cancer, the cancer will eventually recur. This is usually diagnosed by a consistent rise in PSA levels.
Some men will only be diagnosed when the cancer is already at an advanced stage when the cancer has spread to other parts of the body This is called de novo or metachronous disease.
Androgens are male sex hormones. The main one that we are all familiar with is testosterone, but testosterone is broken down or converted into other hormones which work on different parts of the body. In the prostate it’s dihydrotestosterone that affects the functioning of the prostate. To keep things simple we’ll refer to the various androgens as testosterone.
Testosterone is produced mainly in the testes, although a small amount is also produced by the adrenal glands. Unfortunately testosterone is what fuels the growth of prostate cancer cells, so once prostate cancer spreads, the only way to slow the growth of the cancer cells, is to deprive them of testosterone. This is called androgen deprivation therapy (ADT). ADT is sometimes also referred to as hormone therapy. ADT is the mainstay for treating metastatic prostate cancer and it is used alone or in combination with other treatments.
Unfortunately, ADT means that all the good things that testosterone normally does in the adult male body are affected. In order to understand the impact of removing most of the body’s testosterone it is important to have a basic understanding of its role and function in the body.
The role of testosterone and the effects of low testosterone levels
| Function of testosterone in adult men | Result of low testosterone |
| Gives a man his sex drive | Low sex drive |
| Causes spontaneous night time and waking erections | Loss of spontaneous night time and waking erections |
| Provides men with energy and drive | Loss of energy and drive |
| Provides men with a general sense of wellbeing and helps with mental functioning | Depression and lack of mental sharpness |
| Regulates the functioning of the internal sex organs responsible for sperm production, orgasm and ejaculation | Low fertility and reduced orgasmic and ejaculatory function |
| Maintains lean muscle mass | Loss of lean muscle mass and
Increased abdominal obesity Obesity leads to an increased risk for high cholesterol , cardiovascular disease and type 2 diabetes |
| Maintains muscle strength | Loss of muscle strength and reduced athletic performance |
| Promotes bone density | Increased risk for osteoporosis and pathological fractures |
Androgen deprivation therapy (ADT)
Once advanced prostate cancer is diagnosed, androgen deprivation therapy (ADT) is usually initiated to stop testosterone production by the testes. Advanced prostate cancer that has never been treated with (ADT) is referred to as hormone sensitive metastatic prostate cancer (mHSPC) or castrate sensitive prostate cancer. The objective of ADT is to reduce testosterone levels to below 1.73nmol/l. This is referred to as castrate levels of testosterone.
| Normal testosterone levels | 12 to 40 nmol/l |
| Intermediate testosterone levels | 8 to 12 nmol/l |
| Low testosterone levels | <8 nmol/l |
| Castrate testosterone levels | <1. 7 nmol/l |
There are two ways to reduce testosterone to castrate levels:
Surgical Castration (orchidectomy)
The removal of the testicles is still commonly used as a form of androgen-deprivation therapy (ADT) within public sector hospitals in South Africa, as it is cost effective and does not require patients having to take medications on an ongoing basis. The main disadvantage is that the procedure is irreversible. It is a simple procedure that can be performed under local anaesthetic.
Chemical castration
This involves the use of medication (injections or tablets) to block the production of testosterone.
In men with symptoms caused by metastatic prostate cancer, treatment is usually started immediately. In men who have a rising PSA but no symptoms from the cancer spreading and no signs showing on imaging tests (biochemical recurrence), there are different approaches. Beginning hormone therapy immediately can help to reduce or delay some of the debilitating symptoms of metastatic prostate cancer like spinal cord compression, pathological fractures and urethral obstruction. However this decision has to be weighed up against the impact of ADT on a man’s quality of life, so some men may prefer to delay treatment until they begin to experience symptoms (see section on side-effects of hormone therapy/androgen- deprivation therapy). Men will need to make an informed decision based on their particular circumstances and preferences.
In addition to ADT, other treatments may be administered as part of the first line treatment strategy. This is now recognised as the standard of care and includes ADT combined with chemotherapy or one of the new second generation antiandrogens. In some cases, ADT may be combined with both of these (triplet therapy). These options are discussed in more detail further on.
Androgen deprivation therapy (ADT) medications
Luteinising hormone-releasing hormone agonists (LHRH agonists)
Administration – by depot injections or a small implant injected under the skin
LHRH agonists available in South Africa: goserelin, triptorelin and leuprorelin acetate
Given 1, 3 or 6 months depending on which medication is prescribed
This medication works by blocking the release of luteinising hormone (LH) which leads to a reduction of testosterone that is equivalent to surgical castration. However, at the start of treatment they can cause an initial surge in testosterone production. This can result in tumour flare which can cause a temporary worsening of symptoms, particularly in patients with spinal metastases who are at risk of spinal cord compression and in patients with bladder neck obstruction. This can be avoided by using an antiandrogen medication together with the LHRH agonist during the first 4 to 6 weeks of treatment.
Gonadotropic –releasing hormone antagonists (GnRH).
Administration – by depot injections
GnRH medications: Degarelix
These medications inhibit LHRH release without causing an initial surge in testosterone which can lead to tumour flare. Testosterone levels drop within a day after having the injections.
Some studies suggest that GnRH medications may cause less cardiovascular side effects than LHRH agonists. They also allow for the rapid return of testosterone to normal levels, which is particularly useful if men are undergoing intermittent hormonal therapy.
Continuous versus Intermittent androgen deprivation therapy
This treatment involves intermittent periods of active treatment with ADT followed by periods of no treatment to allow testosterone levels to return to normal. This minimises the side effects caused by continuous ADT and improves quality of life during the “non-treatment” periods. There is also some evidence that this form of treatment may delay the onset of castrate resistant prostate cancer. This is when the prostate cancer becomes resistant to ADT.
Treatment is given for 6 to 9 months, if there are no clinical signs of the cancer progressing and a PSA <4ng/ml is reached in men with confirmed metastatic prostate cancer, or a level of 0.5ng/ml in men who have relapsed after treatment for localised or locally advanced prostate cancer.
Treatment is then stopped to allow testosterone levels to return.
The PSA is strictly monitored and treatment is resumed if it rises.
10-20ng/ml is used as the threshold for men with confirmed metastatic prostate cancer and a level of 4 to 10ng/ml for men who have relapsed after treatment for localised or locally advanced prostate cancer or if there are clinical signs that he cancer has progressed. This cycle is repeated until the first signs of castration resistance appear.
A GnRH medication may be preferable for this type of treatment as it does not cause tumour flare and it potentially allows testosterone to return to normal levels more quickly than with a LHRH agonist.
Combinations of ADT and other treatments
ADT in combination with first generation antiandrogens
These medications don’t stop testosterone production but instead block the uptake of testosterone by the androgen receptors. They are not as effective as LHRH agonists when used alone. They are most commonly used when initiating treatment with LHRH agonists to prevent tumour flare.
There are 2 types of antiandrogens:
Steroidal antiandrogens (cyproterone acetate)
This drug has a central testosterone lowering effect and can be taken alone, although they are not as effective as LHRH agonists.
Non-steroidal antiandrogens (bicalutamide)
These drugs block the uptake of testosterone at the receptor sites and should not be used alone.
ADT in combination with chemotherapy
For men with high volume metastatic prostate cancer, ADT alone is no longer considered to the standard of care. It is recommended that it be combined with chemotherapy or one of the new second generation antiandrogens.
Docetaxel is a form of chemotherapy, and it has been shown to be more effective at delaying cancer progression and prolonging life than just ADT alone in men with hormone sensitive prostate cancer. The benefit appears to be the greatest in men who have high volume metastatic prostate cancer. A man is considered to have high volume prostate cancer if he has a visceral metastasis (cancer that has spread to soft tissue organs such as the lungs, liver etc) or if he has 4 or more bone lesions, one of which is beyond the vertebrae or pelvis.
Chemotherapy may not be an option in men who are frail as it can cause a variety of toxic side effects. Patients must have frequent blood count tests to monitor for neutropenia which can compromise the body’s ability to fight infections.
ADT in combination with second generation antiandrogens
ADT alone is no longer considered to be standard of care and the latest international guidelines now recommend that ADT should be combined with chemotherapy for patients with high volume prostate cancer or with one of the new second generation antiandrogens. This combination treatment prolongs life for a longer period than ADT alone. It also helps to delay symptoms and the progression of the disease to a castrate resistant state.
ADT in combination with Abiraterone acetate
Abiraterone acetate was the first 2nd generation antiandrogen. It blocks an enzyme which stops testosterone production in the testes, adrenal glands and cancer cells. It still needs to be taken together with ADT, and is given with low-dose corticosteroids, because it affects certain functions of the adrenal glands. Patients need to be closely monitored for changes to liver function, blood pressure, potassium levels and for fluid retention.
ADT in combination with Androgen Receptor Pathway Inhibitors
The first of the new androgen receptor pathway inhibitors (ARTA’s) to be launched was enzalutamide, followed by apalutamide and darolutamide. For prostate cancer cells to grow, androgens have to attach themselves to a protein called an androgen receptor inside the prostate cancer cell and then move to the nucleus of the cell in order to produce more cancer cells. These new 2nd generation antiandrogens block this pathway, hence their name. They are still used with ADT. The benefits of combining ADT with ARTA’s, is that they increase life expectancy and delay the progression to castrate resistant prostate cancer. For the best outcomes, they should be given when ADT is started. Because of the improved outcomes of the combination of ADT and the new 2nd generation ARTA’s, ADT alone, is no longer considered standard of care in many developed countries. Recommendations are that they should be combined with one of the 2nd generation antiandrogens for optimal outcomes. However, due to the cost of these new medications this is not always possible within the South African context.
Castrate resistant metastatic prostate cancer and treatment options
Unfortunately most advanced prostate cancers treated with androgen deprivation therapy (ADT) begin to progress again within 12 to 33 months. It is thought that some cancer cells that are not dependant on testosterone begin to develop and so the cancer becomes resistant to androgen deprivation treatment. When prostate cancer becomes resistant to androgen deprivation therapy it is called castrate resistant metastatic prostate cancer (CRPCA).
Most men are diagnosed with castrate- resistant prostate cancer when PSA levels begin to rise despite having castrate levels of testosterone. However men with CRPC can be at very different stages of the disease process. Various tests will help to establish at what stage of the disease process a man is at. Knowing this will help doctors with treatment planning and it will also give an indication as to how long a man might expect to live for. This is referred to as a survival rate.
Further Tests for men with CRPCA
Various tests are used to determine where the cancer has spread to and the extent. Tests may include:
Regular PSA testing
For men with no radiographic signs of the cancer spreading (non- metastatic castrate-resistant prostate cancer) but with a rising PSA level the time that it takes for the PSA to double is highly significant.
Traditional diagnostic imaging tests
Bone scans – These are used to detect cancer that has spread (metastasised) to bone
A CT of the chest, abdomen and pelvis
An MRI in men who can’t have a CT scan.
However these generally only show signs of the cancer spreading in men if the PSA is ≥10 ng/mL.
Next generation diagnostic imaging
Newer imaging tests such as (PMSA) PET CT or PET/MRI scans can detect cancer cells that have spread but are not visible with the older imaging tests.
Measuring circulating tumour cells (CTC’s)
An increasing number of CTC’s at baseline results in shorter overall survival rates.
Changes in CTC’s can also be a response to treatment and associated with longer overall survival.
Genetic testing
Genetic testing can help to identify specific genetic mutations in cells. There are targeted treatments available depending on the type of mutation. The types of genetic tests that are recommended are:
A germline genetic test
Germline mutations occur in a sperm cell or an egg cell and are passed directly from a parent to a child at the time of conception. They are copied into every cell in the body and can be passed from generation to generation. The recommended panel of genes that should be tested are:
mutL homolog 1 (MLH1), mutS homolog 2 (MSH2), mutS homolog 6 (MSH6), and postmeiotic segregation increased 2 (PMS2; for Lynch syndrome); breast cancer susceptibility gene (BRCA) 1; BRCA2; ataxia telangiectasia mutated (ATM); partner and localizer of BRCA2 (PALB2); and checkpoint kinase 2 (CHEK2).
About 5 to 10 percent of patients have germline mutations in DNA mismatch repair genes. These patients can be treated with poly (ADP-ribose) polymerase (PARP) inhibitors.
Next generation sequencing of prostate tumour tissue to identify somatic mutations
These mutations occur from damage to genes in an individual cell during a person’s life. Somatic or acquired mutations are the most common cause of cancer. This type of genetic testing can identify potentially targetable abnormalities for which various drug treatments are available.
| Mutation | Treatment |
| homologous recombination repair [HRR] deficiency | poly[ADP-ribose] polymerase inhibitor |
| deficient mismatch repair [dMMR] or high levels of microsatellite instability [MSI-H] | pembrolizumab |
| rare neurotrophic tyrosine receptor kinase [NTRK] fusions | tropomyosin receptor kinase [TRK] inhibitor |
Treatments for castrate resistant prostate cancer
Continuation of androgen deprivation therapy
In most cases ADT can be continued whilst other treatments are added. Some of the newer treatments are not available at public sector hospitals due to cost. Medical aids may also not provide full reimbursement for these.
Treatments for men with non-metastatic castrate resistant prostate cancer
This is classified as: (M0 CRPC)
These are men who have a rising PSA but no signs of metastases.
Drugs that work by interfering with androgenic stimulation of prostate cancer cells in conjunction with ADT have been shown to delay disease progression and prolong survival. These include: enzalutamide and apalutamide.
Treatments for men with metastatic castrate resistant prostate cancer
This is classified as: (M1 CRPC)
These are men who have metastases. Various treatments given in conjunction with ADT can prolong life. These include:
Drugs that interfere with androgenic stimulation of prostate cancer cells
These include enzalutamide and apalutamide
Drugs that Inhibit androgen biosynthesis
Abiraterone
Chemotherapy
Chemotherapy is usually reserved for men with prostate cancer that is causing symptoms and where there are signs that the cancer is progressing at a rapid rate
First line chemotherapy with docetaxel
Docetaxel is the first chemotherapy treatment option for men who have metastases and castrate resistant prostate cancer and who are well enough to tolerate treatment. (Various assessment screening questionnaires can be used to determine if a man is likely to be fit enough for this treatment option). It is given every 3 weeks for up to 10 cycles. Treatment is continued, provided men are able to tolerate it and there is no evidence from imaging tests that the disease is progressing.
Second-line chemotherapy with cabazitaxel
Once patients become resistant to treatment with docetaxel, the next option is to use a drug called cabazitaxel.
Alternative chemotherapy treatment
Another option is available for those men who are unable or unwilling to have docetaxel or cabazitaxel. This treatment consists of mitoxantrone plus prednisone and although it doesn’t prolong life, it can help with relieving the symptoms of advanced prostate cancer.
Treatments for bone metastases
In most men who have metastatic prostate cancer, the cancer will spread to bone. The cancer cells interact with the different types of bone cells. Most commonly the interaction is with the bones “builder cells” (osteoblasts) resulting in an abnormal build-up of bone. Less commonly the interaction is with the bones “demolisher cells” (osteoclasts) resulting in soft sections of damaged bone. Some men will have a combination of these interactions. The result is bone pain and an increased risk of fractures (pathological fractures).
Treatment is aimed at:
- slowing the spread of the cancer to bones
- relieving bone pain
- strengthening bones to prevent fractures
Pain medication for bone metastases
Bone pain often starts in the lower back, pelvis and/or hips. It is likely to get worst as the cancer progresses and eventually it usually becomes constant. Everyone has a different ability to tolerate pain, so it’s important to get help when you need it. Different pain medications are available depending on how you are managing.
Initially mild pain killers will help. As pain increases, mild opioids are usually prescribed. For severe pain, strong opioids are generally used. Other medications that are not pain killers can also be helpful. These include antidepressants, sedatives, anti-seizure meds, muscle relaxants and anxiolytics.
Radiotherapy for bone metastases
Focal External beam radiation can help if there only a few sites (See section on external beam radiation). 80% of men report a rapid reduction in pain. Treatment may be for one session only or over 2 to 3 weeks. There are minimal side effects from this type of radiation treatment.
When there are multiple metastases wide-field radiation may be given. This involves the administration of radiation to a large section of the body (from the jaw to the pelvis, from the chest to the pelvis or from the pelvis to the ankles). This treatment can both, slow the progression of existing metastases and the development of new ones. Side effects can include inflammation of the lungs, cataracts, nausea, vomiting and diarrhoea. More rarely, blood cells can be adversely affected.
Bisphosphonates and denosumab for bone metastases
These medications help to slow down the bone damage caused by osteoclasts. These are the bodies bone “demolisher cells” (osteoclasts) which react with prostate cancer cells resulting in soft sections of damaged bone.
Treatment with these medications can help with the symptoms caused by bone metastases as well as helping to delay bone-related events in men with castrate resistant prostate cancer.
Radiopharmaceuticals for bone metastases
This is a rapidly evolving field. Currently in South Africa Radium -223 is available. It is used to treat low-volume bone metastases. It helps by reducing bone pain and delaying fractures.
Treating spinal cord compression
Spinal cord compression caused by bone metastases usually results in low back pain with numbness and weakness in the legs, although any area of the spine may be affected. This may be followed by the loss of bowel and bladder control. A spinal MRI can be used to confirm the diagnosis. Urgent surgery is required to prevent or reduce neurological impairment, gait disturbance and the impact on quality of life. This involves decompressing the vertebra and in some cases stabilization.
External beam radiation and steroids may be used as follow-up treatment.
References
- Kirby RS, Patel M. Fast Facts: Prostate Cancer. Eight Edition 2014. Health Press Limited
- Coetzee L. Fast Facts: Metastatic Prostate Cancer. Health Press Limited 2017
- For Healthcare professionals: Prostate cancer essentials: Hormone therapy. Prostate Cancer UK. Available at: https://prostatecanceruk.org/for-health-professionals.
- Dawson NA et al. Overview of the treatment of castration-resistant prostate cancer (CRPC). In: UpToDate, Post, N V (Ed). UpToDate, Waltham, MA, 2021.
5 Mutambiwa S. Understanding recucrrent and metastatic prostate cancer
