PSA Blood Test or Digital Rectal Examination?
With prostate cancer predicted to be the most common cancer in South Africa (SA) by 2030, more men are choosing to screen for if detected early the cancer is potentially curable. The Prostate Cancer Foundation (PCF) recommends informed patient-based screening in men with a life expectancy more than 10 years in the following situations:
– From the age of 40 in black African men and in men who have a family history of prostate and/or breast cancer in a first degree relative. The reason for recommending screening in black males at a younger age, is that they have a 60% greater risk for prostate cancer and are more than twice as likely to die from the disease.
– From the age of 45 years for all other men
In addition, patients with a history of lower urinary tract symptoms (LUTS) and/or clinical suspicion of prostate cancer, regardless of age group, should be tested, usually with prostate specific antigen (PSA) and a digital rectal examination (DRE).
When looking at these tests it is important to recognize that a positive screening test does not always mean the presence of prostate cancer but rather gives an indication that there may be a problem. There are two factors used to determine the accuracy of a test in medicine:
Sensitivity– the ability to correctly identify patients with the disease (positive predictive value)
Specificity– the ability to correctly identify patients without the disease (negative predictive value)
So let us look at how PSA test DRE shape up as screening tools.
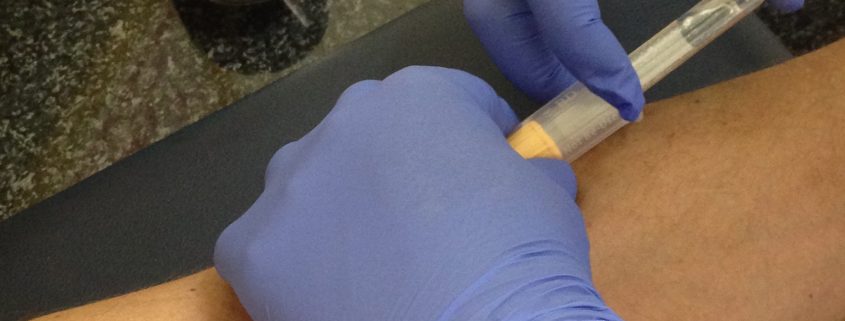
Prostate Specific Antigen (PSA) – is a blood test of a protein normally made in the prostate. PSA levels can increase when there are cancer cells in the prostate. PSA also increases with age as men have natural enlargement of the gland called benign prostatic hyperplasia (BPH) and certain other conditions, such as obesity, and some drugs can lower the PSA which is the reason age reference ranges decide individual management decisions.
Other common conditions that can raise PSA level include:
- inflammation of the prostate (prostatitis)
- urinary tract infection
- prostate cancer
- recent ejaculation
Accuracy of PSA:
The PSA test is far from perfect but at present it is the best we have. Using a cut-off of ≥4.0 ng/ml the PSA has a sensitivity of about 21% and a specificity of about 91%. If the cut-off is reduced to 3.0 ng/ml the sensitivity is about 32% for detection of any prostate cancer and for the detection of a high-grade cancer about 68%. One of the advantages of the PSA test is its ability to pick up prostate cancer 5 to 10 years before it causes symptoms. Because the test is not perfect, even if your PSA is normal there is still a chance that you have prostate cancer.
A Digital Rectal Rectal Examination (DRE) – During a DRE the doctor inserts a gloved, lubricated finger into the rectum to feel the back section of the prostate for enlargement, lumps, or irregularities. The DRE can only detect tumours that are in the area that can be felt by the doctor’s finger, although this is the area where most cancers occur. It may not detect small tumours in the early stages of the disease that the PSA will pick up.
Sensitivity is about 52% and specificity about 59% which are relatively low, which is why some guidelines no longer recommend DRE as a primary screening test for prostate cancer.
Athough PSA is the best screening test we currently have, for optimal detection it should be done together with a DRE. In one large multicentre screening study of 6630 men, the prostate cancer detection rate was 3.2% with DRE as opposed to 4.6% for PSA, and 5.8% when using both tests. So, if you want to be extra sure, have both tests.